Laparoscopic ERCP: Challenges and Solutions in Minimally Invasive Biliary and Pancreatic Procedures
Laparoscopic ERCP: Challenges and Solutions in Minimally Invasive Biliary and Pancreatic Procedures
Introduction:
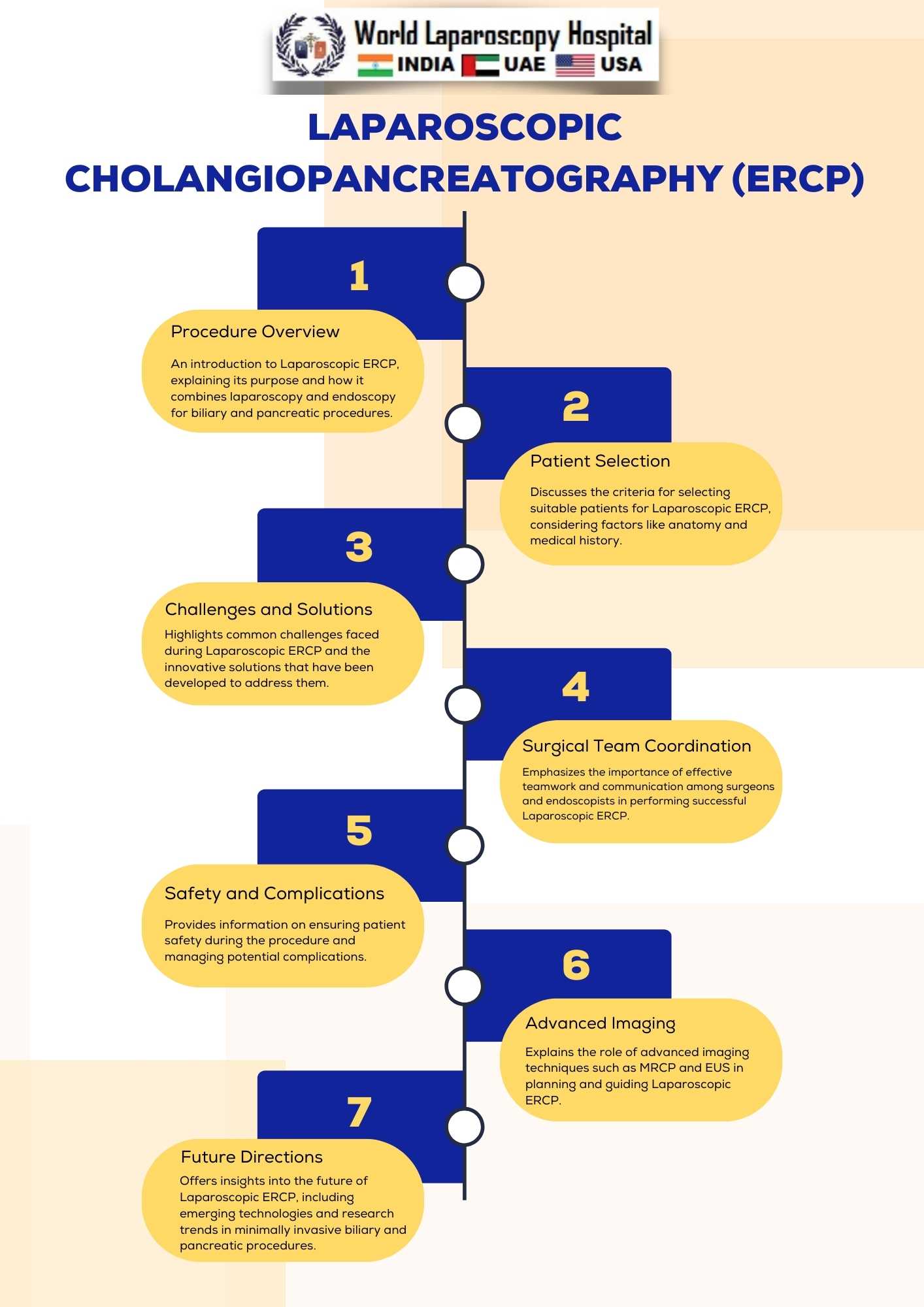
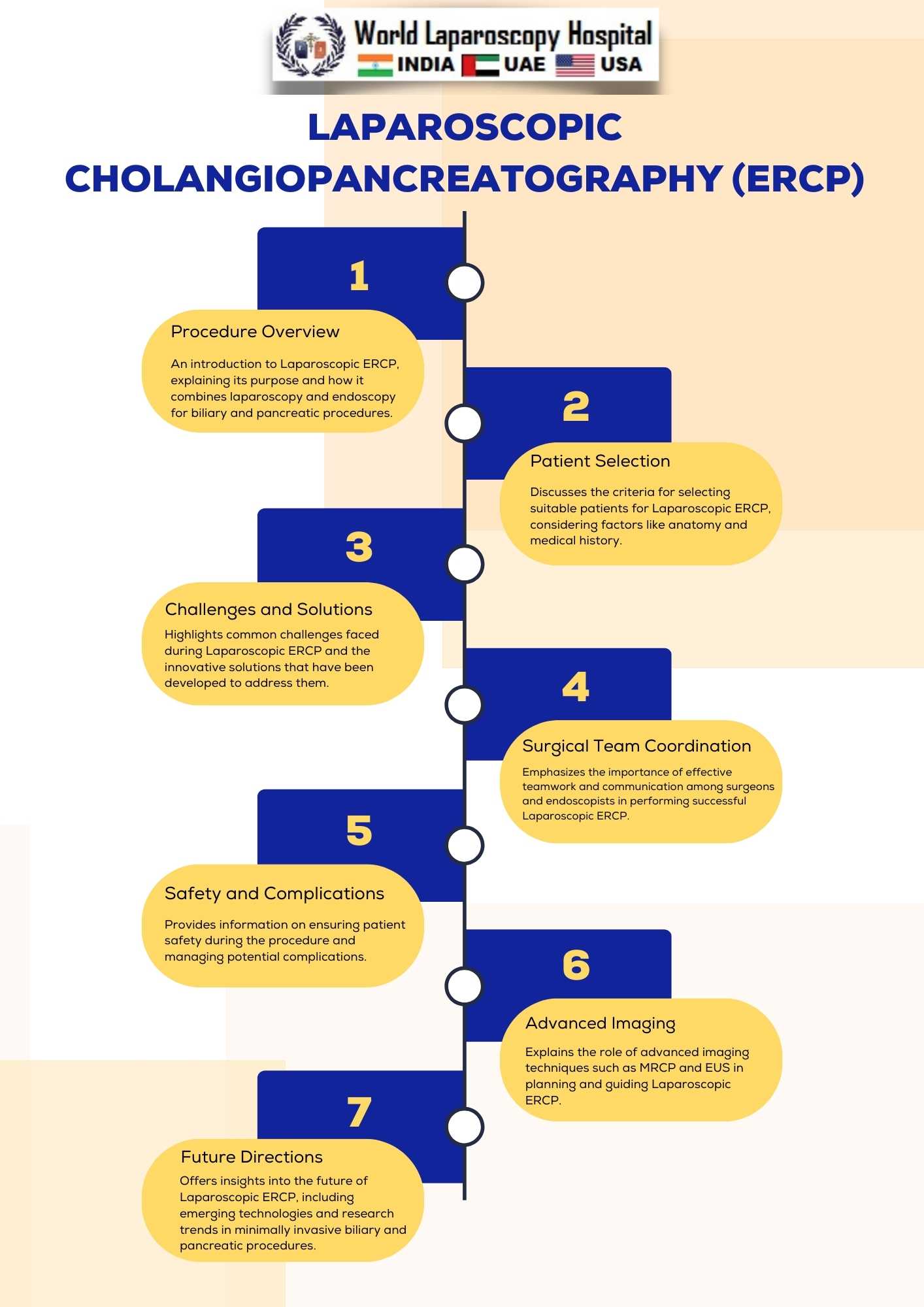
Laparoscopic Endoscopic Retrograde Cholangiopancreatography (ERCP) has emerged as a significant advancement in the field of minimally invasive surgery, particularly in the management of biliary and pancreatic disorders. This innovative approach combines laparoscopy and endoscopy to provide a less invasive alternative to traditional open procedures. While laparoscopic ERCP offers numerous benefits, it also presents unique challenges that require careful consideration and innovative solutions. In this article, we will explore the challenges faced by surgeons when performing laparoscopic ERCP and discuss the solutions that have been developed to overcome them.
Understanding Laparoscopic ERCP
Laparoscopic ERCP is a complex procedure that involves the use of both laparoscopic and endoscopic techniques to diagnose and treat conditions related to the biliary and pancreatic ducts. It is commonly employed in cases of choledocholithiasis, chronic pancreatitis, biliary strictures, and other biliary and pancreatic disorders. The procedure aims to access and visualize the biliary and pancreatic ducts, perform interventions such as stone removal or stent placement, and provide therapeutic relief to patients.
Challenges in Laparoscopic ERCP
1. Access and Visualization Challenges
- Accessing the biliary and pancreatic ducts laparoscopically while maintaining a clear visual field can be challenging.
- Precise positioning of laparoscopic instruments and endoscope is crucial for successful navigation.
- Overcoming anatomical variations and difficult-to-reach areas adds complexity.
2. Coordination of Surgical Team
- Laparoscopic ERCP requires effective coordination between the surgical team, including laparoscopic surgeons and endoscopists.
- Teamwork and communication are essential for smooth execution.
3. Patient Selection
- Proper patient selection is crucial, as not all patients are suitable candidates for laparoscopic ERCP.
- Factors like obesity, previous abdominal surgeries, and complex anatomy can affect the feasibility of the procedure.
4. Learning Curve
- Surgeons need to overcome a steep learning curve when transitioning to laparoscopic ERCP.
- Mastery of both laparoscopic and endoscopic techniques is necessary for success.
5. Complications and Safety
- Complications such as bile duct injuries, pancreatitis, bleeding, and infection must be managed effectively.
- Ensuring patient safety is a top priority.
Solutions in Laparoscopic ERCP
1. Advanced Imaging Techniques
- Preoperative imaging, including Magnetic Resonance Cholangiopancreatography (MRCP) and Endoscopic Ultrasound (EUS), aids in understanding the patient's anatomy and planning the procedure.
2. Robotic-Assisted Surgery
- Robotic platforms offer enhanced dexterity and precision, addressing some of the challenges of laparoscopic ERCP.
3. Dedicated Training and Education
- Surgeons should undergo specialized training programs to acquire the necessary skills for laparoscopic ERCP.
- Mentorship and proctoring can help shorten the learning curve.
4. Patient-Specific Planning
- Comprehensive patient evaluation helps identify optimal candidates for laparoscopic ERCP.
- Tailored surgical plans consider individual anatomical variations.
5. Multidisciplinary Approach
- Collaboration between laparoscopic surgeons, endoscopists, and interventional radiologists enhances patient care.
- Regular multidisciplinary meetings can improve decision-making.
6. Continuous Quality Improvement
- Monitoring and analyzing outcomes, including complications and success rates, leads to continuous improvement in laparoscopic ERCP techniques.
7. Minimally Invasive Instruments
- Developments in laparoscopic instruments, including smaller diameter scopes and specialized tools, aid in navigation.
Conclusion:
Laparoscopic ERCP presents a promising avenue for minimally invasive management of biliary and pancreatic disorders. While it comes with its share of challenges, innovative solutions and a commitment to excellence in surgical practice have expanded its applicability and improved patient outcomes. Surgeons must continue to refine their skills, collaborate across disciplines, and embrace technological advancements to maximize the benefits of laparoscopic ERCP while minimizing its challenges. As this field continues to evolve, the future holds great promise for patients and practitioners alike in the realm of minimally invasive biliary and pancreatic procedures.
Introduction:
Laparoscopic Endoscopic Retrograde Cholangiopancreatography (ERCP) has emerged as a significant advancement in the field of minimally invasive surgery, particularly in the management of biliary and pancreatic disorders. This innovative approach combines laparoscopy and endoscopy to provide a less invasive alternative to traditional open procedures. While laparoscopic ERCP offers numerous benefits, it also presents unique challenges that require careful consideration and innovative solutions. In this article, we will explore the challenges faced by surgeons when performing laparoscopic ERCP and discuss the solutions that have been developed to overcome them.
Understanding Laparoscopic ERCP
Laparoscopic ERCP is a complex procedure that involves the use of both laparoscopic and endoscopic techniques to diagnose and treat conditions related to the biliary and pancreatic ducts. It is commonly employed in cases of choledocholithiasis, chronic pancreatitis, biliary strictures, and other biliary and pancreatic disorders. The procedure aims to access and visualize the biliary and pancreatic ducts, perform interventions such as stone removal or stent placement, and provide therapeutic relief to patients.
Challenges in Laparoscopic ERCP
1. Access and Visualization Challenges
- Accessing the biliary and pancreatic ducts laparoscopically while maintaining a clear visual field can be challenging.
- Precise positioning of laparoscopic instruments and endoscope is crucial for successful navigation.
- Overcoming anatomical variations and difficult-to-reach areas adds complexity.
2. Coordination of Surgical Team
- Laparoscopic ERCP requires effective coordination between the surgical team, including laparoscopic surgeons and endoscopists.
- Teamwork and communication are essential for smooth execution.
3. Patient Selection
- Proper patient selection is crucial, as not all patients are suitable candidates for laparoscopic ERCP.
- Factors like obesity, previous abdominal surgeries, and complex anatomy can affect the feasibility of the procedure.
4. Learning Curve
- Surgeons need to overcome a steep learning curve when transitioning to laparoscopic ERCP.
- Mastery of both laparoscopic and endoscopic techniques is necessary for success.
5. Complications and Safety
- Complications such as bile duct injuries, pancreatitis, bleeding, and infection must be managed effectively.
- Ensuring patient safety is a top priority.
Solutions in Laparoscopic ERCP
1. Advanced Imaging Techniques
- Preoperative imaging, including Magnetic Resonance Cholangiopancreatography (MRCP) and Endoscopic Ultrasound (EUS), aids in understanding the patient's anatomy and planning the procedure.
2. Robotic-Assisted Surgery
- Robotic platforms offer enhanced dexterity and precision, addressing some of the challenges of laparoscopic ERCP.
3. Dedicated Training and Education
- Surgeons should undergo specialized training programs to acquire the necessary skills for laparoscopic ERCP.
- Mentorship and proctoring can help shorten the learning curve.
4. Patient-Specific Planning
- Comprehensive patient evaluation helps identify optimal candidates for laparoscopic ERCP.
- Tailored surgical plans consider individual anatomical variations.
5. Multidisciplinary Approach
- Collaboration between laparoscopic surgeons, endoscopists, and interventional radiologists enhances patient care.
- Regular multidisciplinary meetings can improve decision-making.
6. Continuous Quality Improvement
- Monitoring and analyzing outcomes, including complications and success rates, leads to continuous improvement in laparoscopic ERCP techniques.
7. Minimally Invasive Instruments
- Developments in laparoscopic instruments, including smaller diameter scopes and specialized tools, aid in navigation.
Conclusion:
Laparoscopic ERCP presents a promising avenue for minimally invasive management of biliary and pancreatic disorders. While it comes with its share of challenges, innovative solutions and a commitment to excellence in surgical practice have expanded its applicability and improved patient outcomes. Surgeons must continue to refine their skills, collaborate across disciplines, and embrace technological advancements to maximize the benefits of laparoscopic ERCP while minimizing its challenges. As this field continues to evolve, the future holds great promise for patients and practitioners alike in the realm of minimally invasive biliary and pancreatic procedures.
2 COMMENTS
Dr. Vishey Patil
#1
Nov 26th, 2023 8:49 am
Laparoscopic Endoscopic Retrograde Cholangiopancreatography (ERCP) marks a pivotal advancement in minimally invasive surgery for biliary and pancreatic disorders. This article explores the benefits, challenges, and innovative solutions in performing laparoscopic ERCP, providing valuable insights for surgeons.
Dr. Eric Wertz
#2
Dec 3rd, 2023 10:22 am
Laparoscopic Endoscopic Retrograde Cholangiopancreatography (ERCP) is a groundbreaking minimally invasive approach for managing biliary and pancreatic disorders, combining laparoscopy and endoscopy. Explore the benefits, challenges, and innovative solutions in this comprehensive article.
| Older Post | Home | Newer Post |





