DR. MOHAMMAD FAROOQUE
2. Use mosquito forceps to dilate the obliterated Vitello intestinal duct (Scandinavian technique).
3. Insert the 10 mm cannula with trocar with guarded screwing movement, perpendicular to the abdominal wall till give away sensation is perceived.
4. Remove the trocar and push the cannula in.
5. Introduce the 30-degree telescope in after white balancing and focussing at 10 cm distance and visualise the area directly under the port for presence of any bleeding or injury.
6. Transilluminate the abdominal wall and insert one 10 mm port on the left and one 5mm port on the right under vision by the Baseball Diamond concept. You can also use the ipsilateral port with a 7.5 cm distance in between.
7. Do a complete examination of the abdomen and pelvis and push the bowel above the sacral promontory.
8. If the patient has a uterus that is affecting exposure, it can be retracted with a stitch to the anterior abdominal wall.
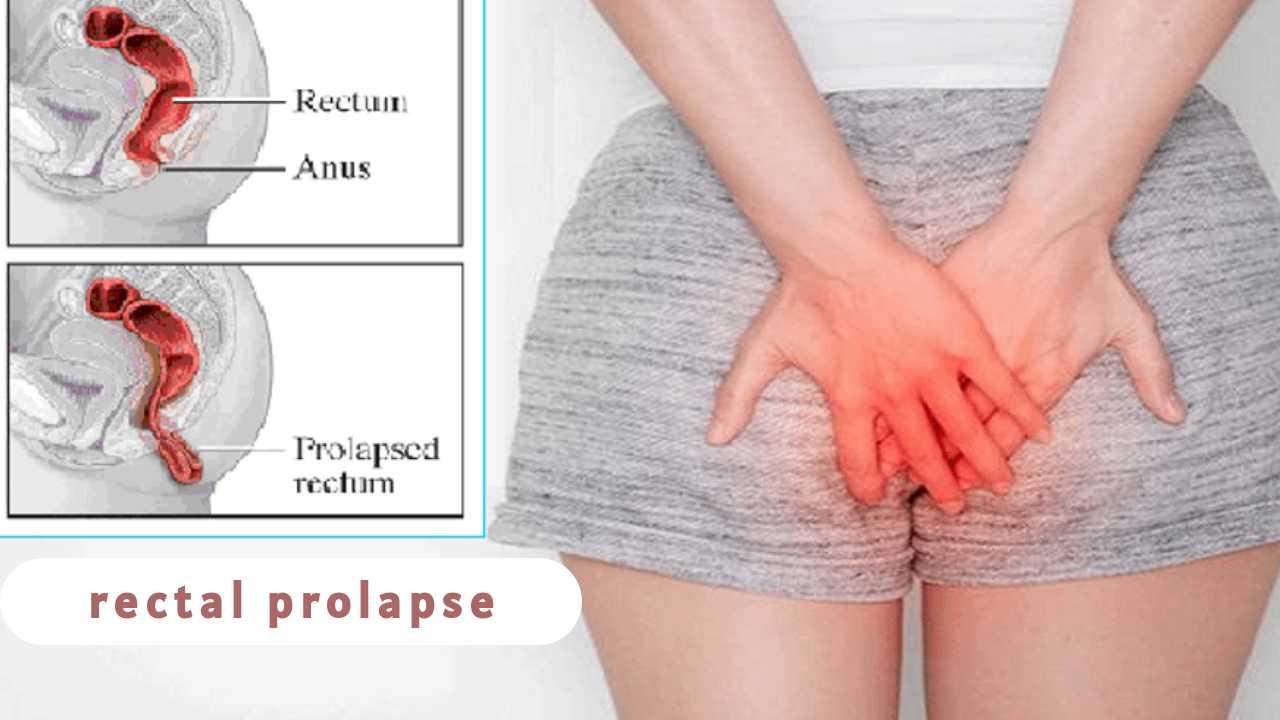
9. Dissection is started posteriorly(Holy plane of Heald). The plane between the mesorectum and retroperitoneum is identified; the retroperitoneum is usually whiter than the mesorectum.
10. A harmonic scalpel is used to enter the posterior pelvic plane under the superior rectal artery, and the left ureter and hypogastric nerve plexus are identified.
11. Dissection is extended downward through the presacral anatomic space, all the way to the pelvic floor.
12. The dissection must be carried below the rectosacral (Waldeyer) fascia. Often, to facilitate exposure, the right lateral stalk of the rectum is also mobilized.
13. Once the right stalk and posterior areas are mobilized, dissection proceeds anteriorly into the rectovaginal plane.
14. Subsequently, the rectum is mobilized anteriorly to the upper limit of the vagina. During this approach, the nervi erigentes and left lateral ligament are spared.
15. The rectum is then pulled out of the pelvis, and where the fixation will occur is assessed.
16. A window is made on the left side of the rectum to facilitate the rectopexy and dissection on sacral promontory is done to expose it.
17. Posterior placement of mesh approximately of size 12*8 cm is done inserted via the right-lower-quadrant port and is placed all the way down to the pelvic floor, extending cephalad behind the mesorectum.
18. The mesh should cover the posterior part of rectum and some of the lateral stalks of rectum.
19. An overly tight pexy must be avoided to prevent obstruction of the rectosigmoid junction. If suturing is chosen, then use Ethibond suture.
20. It is important to identify the sacral venous plexus before tacking or suturing. The bony promontory and presacral fascia is the ideal location for fixation.
21. Then the mesh is fixed on right and left lateral stalks of rectum with the sutures.
22. Close the fold of peritoneum by continuous intracorporeal suturing so that the mesh is extraperitonealised. You can also use Dundee jamming knot with Aberdeen termination. Care should be taken not to include the mesh while suturing the peritoneum.
23. Desufflation of abdomen done
24. Ports are withdrawn under direct visualisation and optical cannula is withdrawn by sliding over the telescope.
25. Skin incisions are either sutured or stapled.
26. Abdomen is cleaned.
27. Antiseptic dressing done
28. Post-op vitals are noted and the patient is shifted to the recovery room.
Elaborated Steps
Position the patient in the lithotomy position.
Administer general anesthesia.
Secure the endotracheal tube.
Place a Foley catheter.
Preoperative antibiotics are administered.
The abdomen is insufflated using CO2.
The laparoscope is inserted through a 10mm port at the umbilicus.
Place 3-4 additional trocars as required.
The small intestine is retracted to expose the retrorectal area.
The rectum is mobilized by incising the peritoneal reflection.
Mobilize the sigmoid colon by dividing the white line of Toldt.
Identify the sacral promontory.
Dissect behind the rectum to create a tunnel that extends from the sacral promontory to the levator ani muscles.
Insert the mesh into the tunnel created behind the rectum.
Anchor the mesh to the sacral promontory using non-absorbable sutures.
Anchor the mesh to the levator ani muscles using non-absorbable sutures.
Check the position of the mesh to ensure that it is correctly placed and not twisted.
Retract the mesh to ensure that it is taut and not loose.
Inspect the mesh for any defects or tears.
Remove the laparoscope.
Close the ports.
Deflate the abdomen.
Remove the trocars.
Close the incisions with sutures or staples.
Apply sterile dressing to the incisions.
The patient is awakened from anesthesia.
Extubate the endotracheal tube.
Move the patient to the post-anesthesia care unit.
Administer analgesics for pain management.
Monitor vital signs and urine output.
Check the dressing for bleeding or drainage.
Observe the patient for any signs of infection or complications.
Initiate a clear liquid diet.
Remove the Foley catheter once the patient is able to void.
Discharge the patient when stable.
Instruct the patient on postoperative care.
Prescribe antibiotics and analgesics as needed.
Instruct the patient to avoid strenuous activity for 2-4 weeks.
Advise the patient to eat a high-fiber diet and drink plenty of fluids.
Advise the patient to avoid constipation and straining during bowel movements.
Schedule a follow-up appointment.
Evaluate the patient's postoperative course.
Monitor for any complications, such as bleeding or infection.
Evaluate the patient's bowel function.
Adjust medication as needed.
Evaluate the healing of the incisions.
Monitor the patient for any signs of mesh erosion or bowel obstruction.
Recommend physical therapy as needed.
Provide the patient with a detailed report of the procedure and postoperative care.
Advise the patient on any potential complications or side effects of the procedure.
Provide the patient with instructions on follow-up appointments and monitoring.
Advise the patient on when to resume normal activities, such as driving, work, and exercise.
The patient follows up with the surgeon at regular intervals.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment.
The surgeon orders any necessary imaging or laboratory tests to evaluate progress.
The surgeon adjusts medications or treatment as needed.
The surgeon monitors the patient for any signs of complications or side effects.
The surgeon communicates with the patient's primary care physician to ensure continuity of care.
The surgeon provides the patient with information on any further treatment or follow-up care.
The patient continues to follow the surgeon's instructions and attend regular follow-up appointments.
The patient reports any changes in symptoms or complications to the surgeon.
The patient reports any changes in medications or health status to the surgeon.
The surgeon evaluates the patient's healing and progress at each follow-up appointment and provides any further treatment as necessary.
| Older Post | Home | Newer Post |
How to Perform and Implement Task Analysis of Laparoscopic and Robotic Procedures
Task analysis is a critical component of any complex surgical procedure, including laparoscopic and robotic surgeries. It involves breaking down the procedure into its constituent tasks, identifying the steps, skills, and cognitive processes required. Task analysis not only enhances the understanding of these intricate surgeries but also serves as a foundation for training, skill assessment, and continuous improvement in healthcare. In this essay, we will delve into how to conduct and implement task analysis for laparoscopic and robotic procedures.
Understanding the Significance of Task Analysis
Before we explore the procedure for task analysis, it's essential to recognize why it is of paramount importance in the realm of surgery, particularly for laparoscopic and robotic procedures.
1. Enhanced Learning and Training: Task analysis helps in developing structured training programs. It breaks down complex procedures into manageable components, making it easier for trainees to learn and practice each step methodically.
2. Skill Assessment: By understanding the tasks and sub-tasks involved, it becomes possible to assess the competence of surgeons and surgical teams. This is crucial for ensuring patient safety and quality care.
3. Workflow Optimization: Task analysis can reveal inefficiencies in surgical workflows. Identifying these bottlenecks allows for process improvements, potentially reducing surgical times and enhancing outcomes.
4. Error Reduction: Recognizing potential points of error is vital for preventing surgical complications. Task analysis can highlight critical steps where errors are more likely to occur, leading to proactive measures to mitigate risks.
Procedure for Task Analysis of Laparoscopic and Robotic Procedures:
Task analysis for laparoscopic and robotic procedures involves several steps:
Step 1: Define the Surgical Procedure
Begin by clearly defining the surgical procedure you wish to analyze. Whether it's a laparoscopic cholecystectomy or a robotic prostatectomy, having a specific procedure in mind is essential.
Step 2: Gather Expert Input
Engage experts in the field, including experienced surgeons, nurses, and other surgical team members. Their input is invaluable in identifying and detailing the tasks involved.
Step 3: Identify the Tasks and Sub-Tasks
Break down the surgical procedure into tasks and sub-tasks. For instance, in a laparoscopic cholecystectomy, tasks could include trocar placement, camera insertion, gallbladder dissection, and suturing. Sub-tasks under "trocar placement" might involve choosing trocar sizes, making incisions, and inserting trocars.
Step 4: Sequence the Tasks
Establish the chronological order of tasks. Determine which tasks are dependent on others and identify any parallel processes. Sequencing tasks is essential for understanding the flow of the procedure.
Step 5: Define Task Goals and Objectives
For each task and sub-task, define the goals and objectives. What should be achieved in each step? For instance, in gallbladder dissection, the goal might be to safely detach the gallbladder from the liver while preserving nearby structures.
Step 6: Skill and Equipment Requirements
Specify the skills and equipment required for each task. Consider the level of expertise needed, such as basic laparoscopic skills or advanced robotic manipulation. Document the instruments and technology involved.
Step 7: Cognitive Processes
Identify the cognitive processes involved, such as decision-making, spatial orientation, and problem-solving. Understanding the mental aspects of surgery is critical for training and error prevention.
Step 8: Consider Variations and Complications
Acknowledge potential variations in the procedure and anticipate complications. How would the surgical team adapt if unexpected issues arise? Task analysis should encompass both the standard procedure and potential deviations.
Step 9: Develop Training and Assessment Tools
Use the task analysis results to create structured training modules. These modules should align with the identified tasks, objectives, and skill requirements. Additionally, design assessment tools to evaluate the competence of trainees and surgical teams.
Step 10: Continuous Improvement
Task analysis is not a one-time endeavor. Regularly revisit the analysis to incorporate new techniques, technology, and best practices. Continuous improvement is vital for staying at the forefront of surgical care.
Implementing Task Analysis Results:
Once task analysis is complete, it's crucial to implement the findings effectively:
1. Training Programs: Develop and deliver training programs based on the task analysis. These programs should encompass both simulation-based training and real-life surgical experience.
2. Skill Assessment: Use the assessment tools developed during task analysis to evaluate the skills of surgical teams. This can be done through structured evaluations and objective metrics.
3. Quality Improvement: Task analysis can reveal areas for process improvement. Work with the surgical team to implement changes that enhance efficiency and patient outcomes.
4. Error Prevention: Utilize the identified points of error to develop strategies for error prevention. This might involve checklists, preoperative briefings, and enhanced communication protocols.
5. Research and Innovation: Task analysis can also guide research efforts, leading to the development of new techniques and technologies that improve surgical procedures.
In conclusion, task analysis is an indispensable tool in understanding, teaching, and advancing complex surgical procedures such as laparoscopic and robotic surgeries. By meticulously dissecting each task and sub-task, identifying skill requirements, and considering cognitive processes, healthcare professionals can enhance patient safety, optimize surgical workflows, and continually improve the quality of surgical care. Task analysis is not merely an analytical exercise; it is a pathway to excellence in surgical practice.