Laparoscopic Management of Torsion Of Ovary
Dr. Poornima BlagopalConsultant Gynecologist and Robotic Surgeon
Preoperative preparations:
1. Blood investigations and Pre-Anesthetic check-up
2. Crossmatch
3. Informed consent
4. Preoperative Antibiotics
5. Surgical team: Surgeon, Anesthetist, Assistant, Scrubbed nurse
Equipment and Laparoscopy Tower:
1. Monitor (Desirable 26” HD)
2. Light Source and Camera Control Unit (Desirable – LED light source and 3 Chip HD Camera)
3. Insufflators and CO2 Gas Cylinder
4. Electro Surgical Unit (Desirable – High-Frequency Generator)
5. Select Pre-set Pressure (Ideal 12 to 15mmHg)
6. Video Recorder & Printer
7. Suction Irrigation system
8. Veress' needle – 12 cm length
9. Ports: One 10mm reusable port, two 5mm ancillary ports
Laparoscopic set :
. Maryland.
. Laparoscopy Aspiration Needle, Harmonic
. Laparoscopic scissors
. Atraumatic grasping forceps
. Tritome
. Suction Irrigation 5 mm
. Syringe and Normal Saline.
Position of the surgical team and equipment:
1. The surgeon should stand on the left side of the patient and the distance from the screen is 5 times
diagonal length of the screen which is placed opposite and in front of the surgeon.
2. Assistant on the right of the surgeon.
3. Scrub nurse on the left of the surgeon.
4. Anesthetist in the usual position on the head end.
Procedure:
1.Optical port site- supraumbilical (3-4 cms above the umbilicus)
2. Make a stab incision of 2mm with No. 11 surgical blade
3. Check Veress Needle for its spring action and patency
4. Lift up the abdominal wall at the umbilicus and assess its full thickness,
5. Veress Needle is held like a dart at a distance of 4 cm plus the thickness of the abdominal wall from its
distal end.
6. Insertion of veress needle through the incision site in a manner that the veress needle makes an
angle of 90’ with the abdominal wall and an angle of 45’ with the body of the patient, pointing towards
the anus.
8. Insertion is achieved with two audible clicks; first of the Rectus Sheath and second of the
Peritoneum
9. Release the Allis forceps from the Abdominal wall
10. Hold the Veress Needle at an angle of 45’ making sure that no further length of the needle is
advanced.
11. Confirm the intraperitoneal placement of the veress needle by ASPIRATION TEST,
IRRIGATION TEST and HANGING DROP TEST
12. Ensure that the Gas tubing is attached to the Insufflator and the Insufflator is switched ON. This
will remove air from the Gas tubing and fill the gas tubing till its tip with CO2 gas.
13. Confirm Pre-Set Pressure to 15mmHg on the Insufflator
14. Attach the gas tubing to the veress needle and start the flow of CO2gas at 1 liter per minute
15. Confirm obliteration of liver dullness and generalized distension of abdominal wall
16. Keep watch on patient’s vital parameters and EtCO2 readings during insufflation
18. The total amount of gas and actual pressure should rise in a linear fashion.
19. When actual pressure has reached pre-set pressure and amount of gas used might vary between
1.5 to 6 liters for an averagely build young patient
20. Once the pressure reaches the pre-set pressure, remove the veress needle and use size 11 blade to
make skin incision to fit a 10mm port. This can be prechecked by placing a 10mm port on the skin for estimation of incision size
21. Insert the 10mm cannula with trocar by oscillatory screwing motion, the direction being
perpendicular till give way sensation is perceived and then change the direction towards the pelvis.
Once you are in, the trocar should be removed and the telescope should be inserted to confirm the
intraperitoneal placement
22. Connect the insufflator to the optical port and switch on the gas.
23. To begin with, an overview inspection of the entire abdomen must be done and noted.
24. Then reach out to the target organ (ovary of affected side), just about to touch it with the tip
of the telescope, and trans-illuminate the anterior abdominal wall to delineate the site of the target.
25. Use the baseball diamond concept to mark the position of the additional 5 mm ports.
26. 15 to 30 degree Trendelenburg tilt aids in moving the bowel to the upper abdomen.
27. The surgeon must use transillumination to avoid any vessel injuries in prospective port sites. Use the
size 11 blade to make small incisions to fit the 5mm ports at the pre-marked sites as per Baseball
diamond concept.
28. Insert both the 5mm ports under direct vision and using principles same as that used for the primary
port to avoid inadvertent visceral and vascular injuries.
29. The uterine manipulator can be used to lift up the uterus for proper visualization.
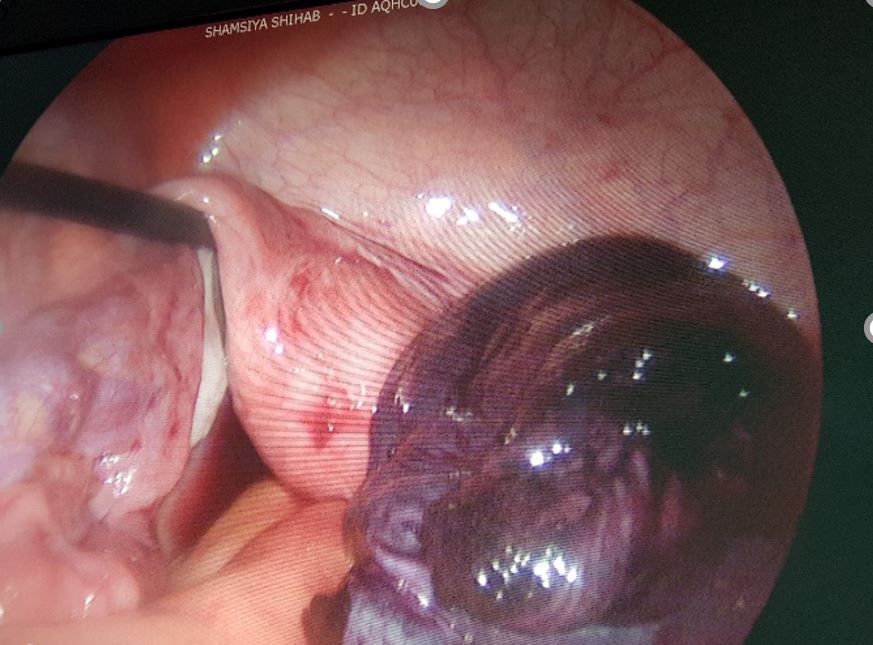
28. Grasp the ovary which has undergone torsion with an atraumatic grasper and with tritome puncture the cyst and aspire the contents.
29. Undo the torsion with the help of 2 graspers.
30. Wait for 3-5 minutes for the blood supply to return.
31. If the color changes to pink, then remove the cyst wall and plicate the round ligament so as to prevent further torsion in the future
32. If there is no color change, then the ovarian tissue has become gangrenous and has to be removed and so proceed with oophorectomy.
33. Clean the peritoneal cavity with suction irrigation.
34. After ensuring complete hemostasis, deflate the abdomen, remove the ancillary port under the vision and the primary port removed along with trocar.
35. Primary port (10 mm) has to be closed with 2-0 vicryl or monocryl.
Thanks for posting this excellent task analysis of Laparoscopic Management of Torsion of Ovary.
| Older Post | Home | Newer Post |
How to Perform and Implement Task Analysis of Laparoscopic and Robotic Procedures
Task analysis is a critical component of any complex surgical procedure, including laparoscopic and robotic surgeries. It involves breaking down the procedure into its constituent tasks, identifying the steps, skills, and cognitive processes required. Task analysis not only enhances the understanding of these intricate surgeries but also serves as a foundation for training, skill assessment, and continuous improvement in healthcare. In this essay, we will delve into how to conduct and implement task analysis for laparoscopic and robotic procedures.
Understanding the Significance of Task Analysis
Before we explore the procedure for task analysis, it's essential to recognize why it is of paramount importance in the realm of surgery, particularly for laparoscopic and robotic procedures.
1. Enhanced Learning and Training: Task analysis helps in developing structured training programs. It breaks down complex procedures into manageable components, making it easier for trainees to learn and practice each step methodically.
2. Skill Assessment: By understanding the tasks and sub-tasks involved, it becomes possible to assess the competence of surgeons and surgical teams. This is crucial for ensuring patient safety and quality care.
3. Workflow Optimization: Task analysis can reveal inefficiencies in surgical workflows. Identifying these bottlenecks allows for process improvements, potentially reducing surgical times and enhancing outcomes.
4. Error Reduction: Recognizing potential points of error is vital for preventing surgical complications. Task analysis can highlight critical steps where errors are more likely to occur, leading to proactive measures to mitigate risks.
Procedure for Task Analysis of Laparoscopic and Robotic Procedures:
Task analysis for laparoscopic and robotic procedures involves several steps:
Step 1: Define the Surgical Procedure
Begin by clearly defining the surgical procedure you wish to analyze. Whether it's a laparoscopic cholecystectomy or a robotic prostatectomy, having a specific procedure in mind is essential.
Step 2: Gather Expert Input
Engage experts in the field, including experienced surgeons, nurses, and other surgical team members. Their input is invaluable in identifying and detailing the tasks involved.
Step 3: Identify the Tasks and Sub-Tasks
Break down the surgical procedure into tasks and sub-tasks. For instance, in a laparoscopic cholecystectomy, tasks could include trocar placement, camera insertion, gallbladder dissection, and suturing. Sub-tasks under "trocar placement" might involve choosing trocar sizes, making incisions, and inserting trocars.
Step 4: Sequence the Tasks
Establish the chronological order of tasks. Determine which tasks are dependent on others and identify any parallel processes. Sequencing tasks is essential for understanding the flow of the procedure.
Step 5: Define Task Goals and Objectives
For each task and sub-task, define the goals and objectives. What should be achieved in each step? For instance, in gallbladder dissection, the goal might be to safely detach the gallbladder from the liver while preserving nearby structures.
Step 6: Skill and Equipment Requirements
Specify the skills and equipment required for each task. Consider the level of expertise needed, such as basic laparoscopic skills or advanced robotic manipulation. Document the instruments and technology involved.
Step 7: Cognitive Processes
Identify the cognitive processes involved, such as decision-making, spatial orientation, and problem-solving. Understanding the mental aspects of surgery is critical for training and error prevention.
Step 8: Consider Variations and Complications
Acknowledge potential variations in the procedure and anticipate complications. How would the surgical team adapt if unexpected issues arise? Task analysis should encompass both the standard procedure and potential deviations.
Step 9: Develop Training and Assessment Tools
Use the task analysis results to create structured training modules. These modules should align with the identified tasks, objectives, and skill requirements. Additionally, design assessment tools to evaluate the competence of trainees and surgical teams.
Step 10: Continuous Improvement
Task analysis is not a one-time endeavor. Regularly revisit the analysis to incorporate new techniques, technology, and best practices. Continuous improvement is vital for staying at the forefront of surgical care.
Implementing Task Analysis Results:
Once task analysis is complete, it's crucial to implement the findings effectively:
1. Training Programs: Develop and deliver training programs based on the task analysis. These programs should encompass both simulation-based training and real-life surgical experience.
2. Skill Assessment: Use the assessment tools developed during task analysis to evaluate the skills of surgical teams. This can be done through structured evaluations and objective metrics.
3. Quality Improvement: Task analysis can reveal areas for process improvement. Work with the surgical team to implement changes that enhance efficiency and patient outcomes.
4. Error Prevention: Utilize the identified points of error to develop strategies for error prevention. This might involve checklists, preoperative briefings, and enhanced communication protocols.
5. Research and Innovation: Task analysis can also guide research efforts, leading to the development of new techniques and technologies that improve surgical procedures.
In conclusion, task analysis is an indispensable tool in understanding, teaching, and advancing complex surgical procedures such as laparoscopic and robotic surgeries. By meticulously dissecting each task and sub-task, identifying skill requirements, and considering cognitive processes, healthcare professionals can enhance patient safety, optimize surgical workflows, and continually improve the quality of surgical care. Task analysis is not merely an analytical exercise; it is a pathway to excellence in surgical practice.