Single Incision Laparoscopic Surgery
Usually, when a new surgical technique is introduced, the focus will be on the feasibility, safety, and clinical advantage of the method. On the other hand, safety is highly dependent on how easily the new technique can be learned by average surgeons. It is a well-known fact that the implementation phase of new techniques is associated with an increased risk of complications emphasizing the importance of thorough training and education for the operating surgeon. The first report of single incision laparoscopic surgery (SILS) was by Navarra et al. who performed a SILS cholecystectomy in 1997. Since then, there have been many reports regarding the use of single incision laparoscopic surgery for appendectomy, splenectomy, nephrectomy, prostatectomy, colectomy, sleeve gastrectomy, adrenalectomy, and adjustable gastric band. However, there have been no reported randomized clinical trials with a direct comparison between SILS to conventional laparoscopic surgery. Despite the lack of evidence demonstrating any superiority of SILS, it is being increasingly performed unfortunately in a largely unregulated fashion without formal training. Concern has been raised that this new procedure is more technically challenging and is likely associated with a significant learning curve and also its own disadvantage and complication. Single-incision laparoscopic surgery (SILS) is a new technique that has now been utilized in many centers for minimal access surgery. The major difficulty with this new technique is the sacrifice that has to be made in terms of comfort and ergonomics. One of the great advantages of SILS is patients are very satisfied with their single scar, and particularly enthusiastic in regard to the cosmetic outcome of the single-incision approach. SILS was first performed for the treatment of appendicitis at the Department of Pediatric Surgery, Dokuz Eylul Medical School, Izmir, Turkey, and first presented at—The Annual Congress of Turkish Association of Paediatric Surgeons, October 2005.
Single-incision laparoscopic surgery
Synonyms
All over world single incision laparoscopic surgery is called by the following names:
• SPL: Single Port Laparoscopy
• SPA: Single Port Access Surgery
• SILS: Single-Incision Laparoscopic Surgery
• LESS: Laparoendoscopic Single-Site Surgery
• OPUS: One Port Umbilical Surgery
• NOTUS: Natural Orifice Transumbilicus Endoscopic Surgery.
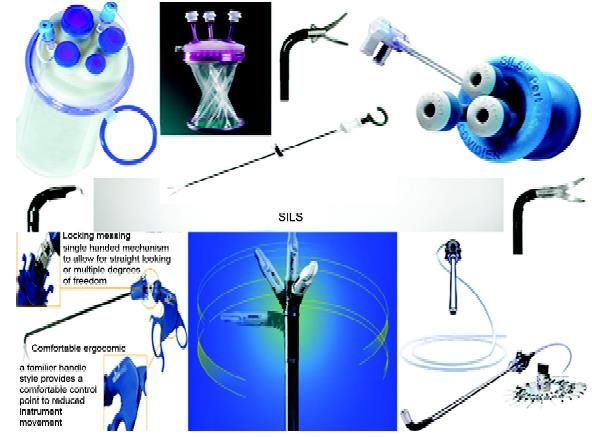
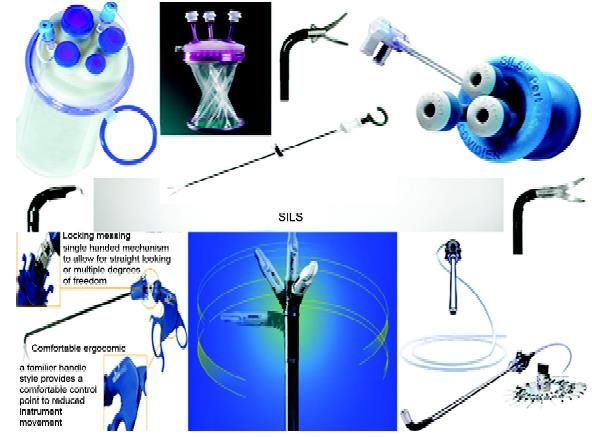
Equipment
Many companies are making single incision laparoscopic surgery equipment. Few of the famous brands are:
• SILS device from: Covidien
• Gel Point system from: Applied Medical
• R-Port and TriPort from: Advanced Surgical Concepts
• Uni-X from: Pnavel.
Case selection is paramount for the success of SILS and at world laparoscopy hospital we performed single incision laparoscopic surgery for the cases which is not complicated and have minimum risk. Good ergonomics in single incision laparoscopic surgery need articulating instruments and high-end energy sources like tissue response generator (LigaSure) and Ultrasonic dissector (Harmonic).
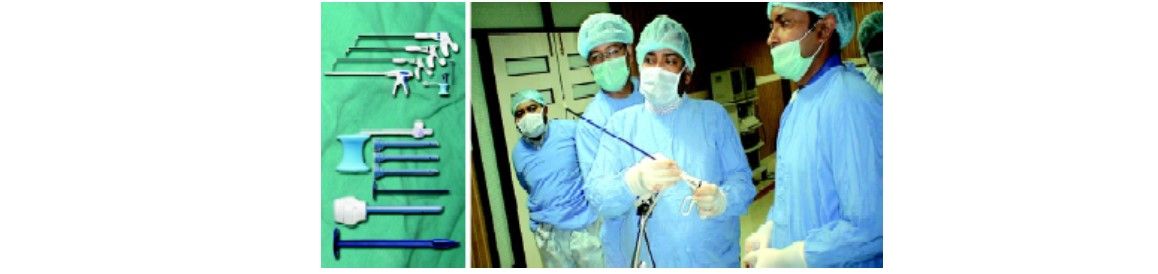
Articulating instruments used in SILS
Some of the popular SILS equipments
Advantage of SILS• Cosmesis +++
• Ease of tissue retrieval ++++
• Combination procedure +++
• Patient acceptance ++++
• Quality of life analysis ++
• Standard equipment ++
• Do not violate natural orifices ++++
• Surgeon’s domain +++

Comparison of scar of SILS and conventional laparoscopic surgery

Comparison of scar of SILS, laparoscopic surgery and open surgery
Disadvantage of SILS
• More pain compared to laparoscopic surgery
• Violating principles of ergonomics
• Incisional hernia chances are more compared to laparoscopic surgery
• More wound infection compared to laparoscopic surgery
• Bigger learning curve compared to laparoscopic surgery
• Not cost-effective compared to laparoscopic surgery.
The evolution of surgery toward less invasive approaches has acted as a stimulant effect towards the development of new less invasive techniques in entering the abdominal cavity. An example of such a technique is the use of a single skin incision through which multiple instruments can be inserted into the abdomen. This single-incision laparoscopic technique has been described by a variety of names as we have discussed earlier. With this single incision of entry, Single-incision laparoscopic surgery (SILS) is a theoretically less invasive approach compared to the standard multi-port laparoscopic surgery. However, SILS may not allow the same level of manual dexterity and technical performance compared to conventional laparoscopic surgery that in a certain aspect, even violates the principle of laparoscopic surgery.

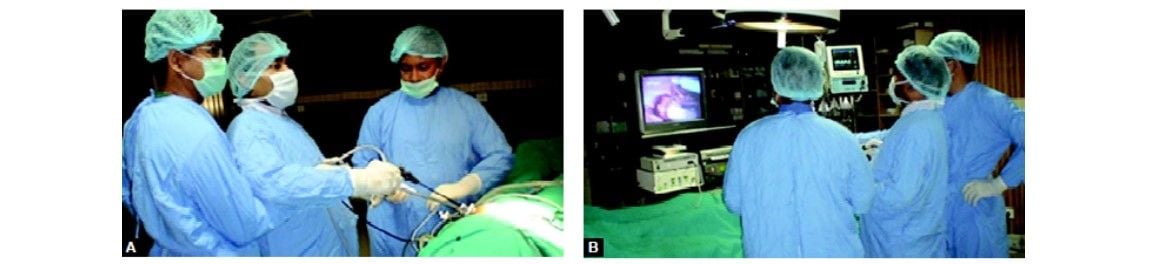
Position of surgical team in SILS
Laparoscopic cholecystectomy has become the standard procedure for treating gallstones, cholecystitis, or gallbladder polyps. Traditionally, LC has involved four ports. Many laparoscopic techniques happen to be developed using this 4- port LC, and it has become possible to do these techniques safely. Now, having established the security of LC, our interest centered on lowering the invasiveness and scarring brought on by the procedure. Cuesta et al. reported single-incision laparoscopic cholecystectomy (SILS), in which two 5 mm ports were introduced through the umbilicus, along with a Kirschner wire hook was introduced with the right subcostal area to pull in an upright direction in order to visualize Calot’s triangle.
Several surgeons have described performing single-incision laparoscopic cholecystectomy using three 5 mm ports in the umbilicus. Meanwhile, Merchant et al. also performed SILS by inserting a Gelport (Applied Medical, Rancho Santa Margarita, CA, USA) to stretch the umbilical fascia incision for simple access with instruments into the abdominal cavity. Furthermore, a method involving several transumbilical- placed ports for single-incision laparoscopic surgery was newly developed, and SILS by way of the ASC Triport (Advanced Surgical Concepts, Wicklow, Ireland) continues to be described successively. On the other hand, a fascinating new instrument named SPIDER (TransEnterix, Inc., Research
Triangle Park, NC) to be used in single-incision surgery was created, and it is used in SILS in an animal experiment has been reported. As a result of these clinical studies, using single-incision laparoscopic cholecystectomy has spread rapidly. Various ports and instruments are available, and various surgical methods utilized in performing SILS can be found in many institutions; however, it is necessary to develop a great method that can be performed safely such as the conventional 4-port LC, and it is also essential to balance safety, operability, and economy in this new technique.
Under general anesthesia, an approximately 25 mm vertical skin incision is made through the center of the umbilicus, the peritoneal cavity should be entered with the open method, and then the SILS port inserted. Three exclusive 5 mm ports were inserted through the SILS port, and one 5 mm port changeable for an exclusive 12 mm port. The pneumoperitoneum should set at 12 to 15 mm and flexible scope (Olympus, Tokyo, Japan) should be used if possible for that intra-abdominal visualization. A couple of loop-type retractors (Miniloop retractor II; Covidien) should be inserted directly within the right subcostal area. Following the patient should be put into the reverse Trendelenburg position and slightly rotated to the left, the fundus of the gallbladder should tighten by way of this loop-type retractor, and also the gallbladder thereafter suspended. In dissecting the gallbladder, a curved grasper, bipolar forceps, or monopolar hooks should be utilized in the two remaining apertures. The cystic duct and artery should be exposed and clipped having a 5 mm clip applier (EndoClip; Covidien) after which divided with laparoscopic scissors. The gallbladder should be extracted by having an endoscopic retrieval bag (Endocatch GOLD; Covidien).
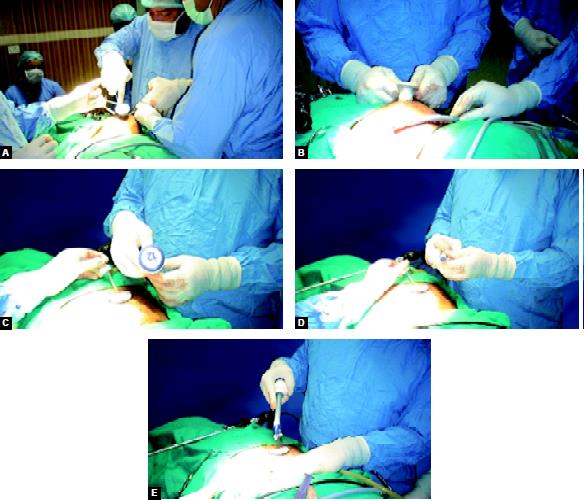
SILS port and its access
Easy replacing a 5 mm port having a 12 mm port is one of the advantages of this port. Actually, SILS while using SILS Port was proven as safe as conventional 4-port LC, and complications for example bile duct injury or uncontrolled bleeding did not occur. However, the issue areas where improvements are needed would be that the umbilical scar through the SILS port is larger than that of conventional 4-port LC. Concretely, the umbilical scar length when it comes to conventional 4-port LC involved 15 mm; however, while using SILS port, it was approximately 25 mm, and furthermore in instances where the umbilicus bottom was shallow, the scar may be unexpectedly large. The conflict between your operative instruments and also the scope is inevitable, and also the procedure seemed to be inconvenient to do since the surgeon and also the assistant needed to stand in the same side from the patient.
The fundus from the gallbladder may tighten with the Roeder or Meltzer knot, and so the straight needle was inserted from the abdominal cavity right subcostal abdominal wall. The gallbladder should be elevated by raising this nylon suture, and a good surgical field obtained. The surgeon operated both one instrument and also the 5 mm flexible scope by hand, and the assistant designed a good surgical field such as Calot’s triangle through the traction of the gallbladder utilizing a fine loop retractor and nylon suture. This technique relieved the interference between your surgeon and also the assistant and between your forceps themselves. To extract the exfoliated gallbladder, one 5 mm port should be removed, and an endoscopic retrieval bag should be inserted directly with an original hole, and the gallbladder ended up being extracted.
The fascial defect of the umbilicus incision should be repaired with approximately two stitches, and an intradermal suture should be performed on the skin. It should be noted that during minimal access surgery generally, we do not shave the hair of skin around the port site. If it is required just trimming of hair should be done on the operation table itself. Shaving of hair many hours before the surgery is liable to bring the bacteria on the surface and may increase the chances of skin infection. This method represents noninvasive surgery that mixes low invasiveness with a scarless outcome. The surgeon operates one instrument along with a 5 mm flexible scope, and the assistant pulls or pushes the fine loop retractor and the nylon suture. This straightforward transition is also an advantage of our 2-port technique since it can be created in any case of cholecystitis or intraperitoneal adhesion.
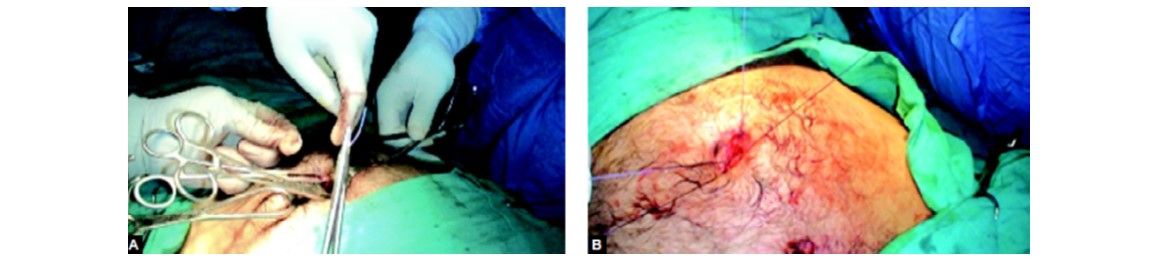
Port closure technique in SILS
With the global growth of using SILS, a large series of cases happen to be reported in many institutes. Curcillo et al. reported within their multi-institutional 297-case series the utilization of one more port away from umbilicus occurred in only 34 cases, plus they concluded that SILS was safe and can serve as an alternative choice to multiport therapy with fewer scars and cosmesis. Erbella and Bunch surprisingly reported their mean operative time was 30 min (from 22 to 75 min) in 100 consecutive SILS cases. Rivas et al. reported that they observed surgeons in training and located that experienced laparoscopic surgeons may not have to undergo a steep learning curve, plus they concluded that SILS was becoming the conventional process of most elective patients with gallbladder disease. Other reports also concluded that SILS was safe; however, Hernandez et al. reported that biliary complication (cystic duct stump leak) took place among 100 SILS cases, and Edwards et al. described that biliary complications occurred in 3.7 percent of the SILS patients (cystic duct stump leak; 1, accessory duct leak; 2). Moreover, iatrogenic combined bile duct and right hepatic artery injury during SILS have already been reported, and the authors recommended that surgeons should have a low threshold to add additional ports at the appropriate interval to make sure that procedures were completed safely, especially in their early stages.
As described, SILS is really a useful technique; however, it is important to make sure that the procedure is as safe as conventional 4-port LC. In our department, to secure the safety, acute cholecystitis is excluded in the indication for SILS for that present. Comparative studies between SILS and conventional 4-port LC regarding operating time, operative cost, complications, postoperative pain, cosmetic result, and time for you to go back to normal activity have been performed gradually with time. Fronza et al. reported that the operating time was significantly longer in SILS, and 12 percent of SILS patients were readmitted within 24 hours after the operation although these readmissions were due to complications similar to those present in 4-port LC. Similarly, Chang et al. figured there is a substantial difference in operative time (SILS was approximately 1.6 times longer) as well as in operative cost (SILS was 1.29 times more expensive), but no difference in postoperative discomfort was observed. However, their result that patients who underwent SILS returned to normal activity 1.8 days earlier than 4-port LC patients seems to demonstrate the usefulness of SILS. Furthermore, two randomized controlled trials (RCTs) that compared SILS with conventional 4-port LC have already been published. One of these trials included 70 patients and the other included 40 patients. Inside a result present with both trials, the operating amount of time in SILS was more than that in 4-port LC, although it was discovered that the two methods differed with regards to the patients’ post-operative pain. According to the conventional reports, the benefit of SILS has not yet become clear; therefore, well-designed RCTs are essential to judge the corrective operative outcomes and also the necessity of SILS.





