Most ovarian abnormalities can be managed la–paroscopically. First laparoscopic salpingo-oophorectomy was performed by Semm in 1984. He reported his experience with a laparoscopic approach to oophorectomy and sal–pingo-oophorectomy.

Figure: Laparoscopic Oophorectomy using bipolar
Laparos–copy may be an alternative of hysterectomy and more conservative management of pain caused by adnexal disease can be performed. If necessary, oophorectomy can be performed laparoscopically with a short hospital stay and recovery period at a later date.
Laparoscopic Anatomy
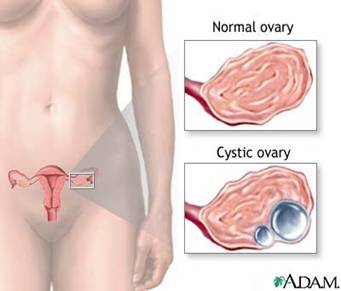
Figure: Anatomy of Ovary
The ovaries are seen clearly by laparoscope because of their whiteness and knobby texture. It is seen more clearly if uterine manipulator is used and uterus is pushed towards anterior abdominal wall. Ovaries hang own in the laparoscopic field. A normal ovary is almond shaped, and approximately 3cm in its greatest diameter.
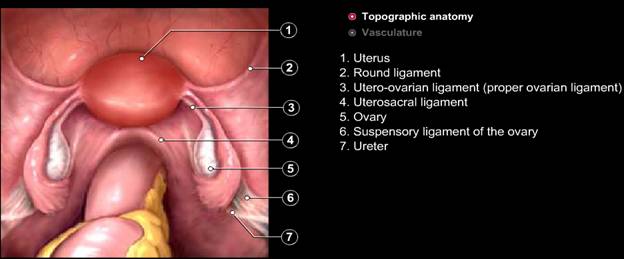
Figure: Normal Pelvis
The ovarian ligaments run from the ovaries to the lateral border of the uterus. Ovary is attached to the pelvic side wall with infundibulopelvic ligament, which carries ovarian artery. One of the common mistakes is injury of the ureter during dissection of the infundibulopelvic ligament. If the uterus is deviated to the contralateral side with the help of uterine manipulator infundibulopelvic ligament is spread out and a pelvic side wall triangle is created. The base of this triangle is the round ligament, the medial side is the infundibulopelvic ligament, and the lateral side is the external iliac artery. The apex of this triangle is the point at which the infundibulopelvic ligament crosses the external iliac artery. The ovarian arteries arise from the aorta to descend lateral to the ureter and genitofemoral nerve. The artery and accompanying vein cross over the external and internal iliac vessels to enter the pelvis. The left ovarian veinjoins the left renal vein and right ovarian vein joins the inferior vena cava.
Laparoscopic Management of Ovarian Cyst
Ovarian cysts are sacs filled with fluid or a semisolid material that develops on or within the ovary. Surgery is indicated if the growth is larger than 4 in (10 cm), complex, growing, persistent, solid and irregularly shaped, on both ovaries, or causes pain or other symptoms. Laparoscopic management of ovarian cyst de–pends on the patient's age, pelvic examination, sonographic images, and serum markers. A large, solid, fixed, or irregular adnexal mass accompa–nied by ascites is suspicious for malignancy. Cul-de-sac modularity, ascites, cystic ad–nexal structures, and fixed adnexae occur with endometriosis and ovarian malignancy. Before selecting any case for laparoscopy, Ca-125 an ovarian cancer marker should be estimated, that may help to identify cancerous cysts in older women. Although ovarian neoplasms can occur at any age, the risk of malignancy is highest during prepu–berty and menopause. Malignancy is not the only concern in managing an ovarian cyst. Patients who wish to preserve their reproductive organ should have the least aggres–sive therapy. In a postmenopausal patient whose fam–ily has a history of ovarian cancer, CA-125 levels may help to detect it in the early stages. However, surgeon should keep in mind that many benign gynecologic disorders are also associated with elevated CA-125 levels, including fibroid uterus, endometriosis, and salpingitis that could lead to unnecessary concern and intervention. Because the risk of malignancy is relatively low in young women, preoperative evaluation should include a history and physical examination. Pelvic ultrasound should be performed to evaluate both ovaries to rule out bilateral endometriomas or teratoma.Hormone levels (such as LH, FSH, estradiol, and testosterone) may be checked to evaluate for associated hormonal conditions. The persistent ovarian cysts must be treated surgically, and evolving laparoscopic tech–nology has enabled endoscopic management of most of them. Although most are benign, the possi–bility of malignancy usually requires a laparotomy using a midline incision. Oral contraceptives have been prescribed for some small cystic adnexal masses in reproductive-aged women on the assumption that decreasing gonadotropin stimulation to a func–tional cyst will hasten its resolution. Either danazol (800 mg/d) or oral contraceptive pills with 50 pg estrogen are advised for any cyst suspected of being functional.
Laparoscopic Anatomy:
Crossing the true brim of pelvis following important tubular structures are found: The round ligament of the uterus, the infundibulopelvic ligament, which contains the gonadal vessels and the ureter. The ovaries and fallopian tube is found between the round ligament and the infundibulopelvic ligament. The ovaries are seen clearly by laparoscope because of their whiteness and knobby texture. It is seen more clearly if uterine manipulator is used and uterus is pushed towards anterior abdominal wall. Ovaries hang own in the laparoscopic field. A normal ovary is almond shaped, and approximately 3cm in its greatest diameter.The ovarian ligaments run from the ovaries to the lateral border of the uterus. Ovary is attached to the pelvic side wall with infundibulopelvic ligament, which carries ovarian artery. One of the common mistakes is injury of the ureter during dissection of the infundibulopelvic ligament. If the uterus is deviated to the contralateral side with the help of uterine manipulator infundibulopelvic ligament is spread out and a pelvic side wall triangle is created. The base of this triangle is the round ligament, the medial side is the infundibulopelvic ligament, and the lateral side is the external iliac artery. The apex of this triangle is the point at which the infundibulopelvic ligament crosses the external iliac artery
Patient Position

Figure: Patient Position for Ovarian Surgery
Patient should be in steep trendelenburg and lithotomy position. One assistant should remain between the legs of patient to do uterine manipulation whenever required.
Port Position
Port position should be in accordance with baseball diamond concept. If the cyst is of right side, one port should be in left iliac fossa and another in right hypochondrium.
Figure: Port Position for right sided ovarian surgery
Operative Procedure
After access the pelvis and upper abdomen have been examined, the cyst contents should be aspirated. Once the capsule is opened, the interior of the capsule is examined and suspicious areas should be sent for biopsy. The entire cyst capsule must be removed to search for an early carcinoma. Whether to per–form oophorectomy or cystectomy depends on the patient's age and characteristics of the mass.
Ovarian Cystectomy
Medical management of endome–triomas has proven ineffective, either laparotomy or operative laparoscopy is necessary Laparoscopic ovarian cystectomy removes the cyst with minimal trauma to the residual ovarian tis–sue. Laparotomy for ovarian cystectomy is not a good procedure because of increased risk of ovarian adhesion formation. Three methods to manage such cysts are drainage, exci–sion and thermal coagulation. By excising the unruptured cyst, histopathologic examination is more complete and the risk of recurrence is mini–mized, but laparoscopic removal of intact cyst is very difficult and aspiration is recommended for functional cysts, which are diagnosed laparoscopically. Many cysts are ruptured during their manipulation despite a delicate technique. Thermal ab–lation does not destroy the entire cyst wall, and the underlying ovarian cortex can be damaged by the heat. Therefore, excision of entire cyst wall with the help of blunt stripping and sharp dissection by scissors are recommended.
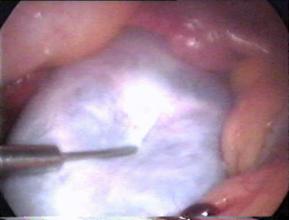
Figure: Ovarian Cyst is aspirated for ovarian cystectomy
The removal of a cyst 10 cm or larger intact is difficult laparoscopically. Aspiration before removal of large cysts is practi–cal and can be accomplished using an 18-gauge laparoscopic needle passed through the separate puncture of abdominal wall while stabilizing the cyst. The suction irrigation instrument can also be used to aspirate the content of the cyst. If gross charac–teristics of ovary look suspicious for malignancy. It is recommended by some of the gynaecologist to perform a peritoneal –washing before puncturing an ovarian cyst, because any cyst may be malignant. The peritoneal fluid or washings should be sent for cytological examination

Figure: Cystic wall is stripped out from ovarian cortex
After aspiration capsule of cyst is stripped from the ovarian stroma using two grasping forceps and the suction-irrigator probe for traction and counter traction. The electrosurgery can be used at low power to seal blood vessels at the base of the capsule and at higher powers to vaporize small remnants of cap–sule. Bipolar forceps also can be used to control bleeding. The Open jaw of bipolar can touch the oozing are and haemostasis can be achieved.

Figure: Cyst is being separated from ovary
Sometimes it is difficult to remove the capsule from the ovarian cortex so that injecting dilute vasopressin between the capsule and cortex facili–tates the stripping procedure. If the cyst wall can–not be identified clearly, the edge of the ovarian incision can be "freshened" with scissors and the resulting clean edge reveals the two layer, Outer layer will be ovarian and inner cystic. If this does not free the capsule, the base of the cyst is grasped, and traction applied to the cyst with counter traction to the ovary. Sometime the complete cyst or portions of the wall may be densely adherent to the ovary, requiring sharp or electrosurgical dissection to completely free the cyst wall. Generally, when the cyst capsule is re–moved from the ovary, the contraction of the ovarian capsule provides significant haemostasis. Bleeding can occur at the base, particularly if the cyst was close to the hilum. Under these circum–stances, a needle electrode or a fine bipolar for–ceps can be used to minimize thermal damage. Large cysts sometime need partial oophorectomy, to remove the distorted portion of the ovary, and the remaining cyst wall can be stripped from the ovarian stroma. Teratoma often can be excised intact but often the cyst rupture. After extraction, if the ovarian edges overlap it self, the defect is left to heal without suturing because adhesions are more likely following the use of suture. In rare instances one or two fine, absorbable monofilament sutures may be needed to approximate the ovarian edges. The sutures are placed inside the ovary to de–crease formation of adhesions.
Endometriomas
Ovarian endometriosis causes the adhesions be–tween the ovarian surface and the broad ligament. As the ovary enlarges, endometriomas form. Sometime surface endometrial implants penetrate more deeply into the cyst wall, making excision more difficult. The degree of endometrial invasion of the cyst wall forms the basis for differ–entiating between these two subtypes and is char–acterized by the progressive difficulty in removing the cyst wall.
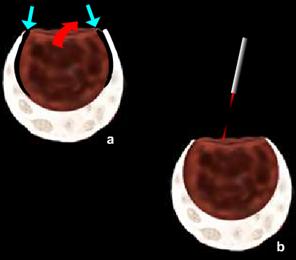
Figure: Deroofing and martipialization for Endometrioma
The least invasive and the technically simplest ap–proach to endometriomas involve laparoscopic fenestration and removal of "chocolate" fluid without cystectomy or ablation of the cyst wall. However, fenestration and irrigation are asso–ciated with a 50% recurrence rate compared to 8% in the group with the capsule removed. Postoperatively, either danazol 800 mg/d or a GnRH analog is used for 6 to 8 weeks. Large hematomas are associated with periovarian adhesions attaching them to the pelvic sidewall and the back of the uterus, and tend to rupture during separation. After mobilizing the ovary, the contents of the cyst are removed with the suction-irrigator probe and the cavity is irrigated. The inside of the cyst is evaluated and the portion of ovarian cortex involved with endometriosis is removed. Using the grasping forceps and the suction-irrigator probe, the cyst wall is grasped and separated from the ovarian stroma by traction and counter traction. Small blood vessels from the ovarian bed and bleeding from the ovarian hilum can be controlled with bipolar electro coagulation. The remaining ovarian tissue is approximated with low-power laser or electrosurgery to avoid adhesions. Low-power, continuous laser or bipolar coagulation applied to the inside wall of the re–dundant ovarian capsule causes it to invert, but excessive coagulation of the adjacent ovarian Stroma must be avoided. Sutures, if needed, are placed inside the capsule and 4-0 polydioxanone sutures used. Fewer sutures result in fewer adhesions. The ability to diagnose and treat endometriosis at earlier stages may prevent its progression and invasion, reducing its adverse impact on health, quality of life, and fertility potential.
Benign Cystic Teratoma
These germ cell tumors occur predominantly in young women. A cystic teratoma contains sebaceous material that is irritating to peritoneal surfaces and can cause chemical peritonitis and possible adhesions. The surgeon should avoid rupturing the cyst. If the cyst is ruptured during excision, it is important to clean the body cavity of all sebaceous material and hair. If rupture at the time of excision, without spending much time, the suction-irrigator is placed in the cyst, the contents aspirated, and the cavity copiously irri–gated. The interior of the cyst is inspected and its lining is grasped and removed from the ovary. The lining is removed from the pelvis through a 10mm port, In case of intact cyst an Endobag may be necessary. A colopotomy can be made through which the cyst is incised and drained and its cap–sule removed. These same procedures can be per–formed through a minilaparotomy incision. The cyst wall is punctured and the contents rapidly aspirated. The wall is removed, placed in an Endo–bag, and removed through the cul-de-sac or through one of the port wound. Following removal, it is critical to irrigate the pelvis copiously with 5 to 10 L of warm lactated Ringer's. The sebaceous mate–rial is less dense than water and will float, facilitat–ing removal. Occasionally, when the cyst is mainly solid, it can be removed intact without rupturing. The cyst wall should be sent for histopatological examination. The pelvis is irrigated with lactated Ringer's solution until all evidence of sebaceous material is re–moved because incomplete removal of this mate–rial can cause peritonitis. During irrigation, the ovarian stroma is inspected to verify haemostasis. If bleeding is present, bleeder points are controlled with a monopolar fulguration or bipolar forceps.

Figure: Extraction of Ovary
If the teratomas are greater than 8 cm, the ovary can be placed in the cul-de-sac adjacent to a colpotomy incision. Cyst is removed transvaginally which minimizes the risk of contamination of upper abdomen and port wound and maintains a minimally invasive approach. The vagina should be cleaned thoroughly and prepared with be–tadine before colpotomy. In elderly women or for those patients in whom the ovary and tube cannot be conserved, salpingo-oophorectomy should be considered. When the cyst wall is benign and the tissue is fragmented, it can be removed through a 10mm suprapubic port. No tissue should be left in the pelvic cavity or on the abdominal wall. Contamination of the anterior abdomi–nal wall should be avoided and if this happens, all tissue must be removed and the incision copiously irrigated and washed. Abdominal wall metastasis has been reported following contamination of the wall during laparoscopy for ovarian cancer.





