Laparoscopic Sigmoidectomy Surgery
Laparoscopic sigmoid colon resection is indicated for both benign (diverticulitis, segmental Crohn's disease, polyp unresectable by colonoscopy) and malignant (primary colon cancer) etiologies, and is one of the most common operations done by laparoscopic methods. In chronic diverticular disease, the indications for laparoscopic sigmoid resection are the same as for open surgery. Sigmoid colectomy for diverticulitis can be technically challenging because of severe inflammation in the left-lower quadrant and pelvis.
Patient Positioning and Operating Room Setup
A proper patient position is key to both facilitating operative maneuvers and preventing complications such as nerve and vein compression, and traction injuries to the brachial plexus. The patient is placed supine, in the modified lithotomy position, with legs abducted and slightly flexed at the knees. The patient's right arm is alongside the body, whereas the left arm is usually placed at a 90° angle. Adequate padding is used to avoid compression on bone prominences. A nasogastric or orogastric tube and a urinary catheter are placed. Adequate thromboembolism prophylaxis should be used, as preferred by the surgeon, and intermittent leg compression stockings can be used as well. The procedure is usually performed with two assistants and a scrub nurse. The surgeon is on the right side of the patient and the second assistant is also on the right side. The first assistant stands between the patient's legs and the scrub nurse at the lower right side of the table. The team remains in the same position throughout the entire procedure. It is advisable to use a table that can be easily tilted laterally and placed into steep Trendelenburg and reverse Trendelenburg position, in order to facilitate exposure of the pelvic space and of the splenic flexure. The laparoscopic unit with the main monitor is located on the left side of the table. It is useful to use a second monitor placed above the patient's head.
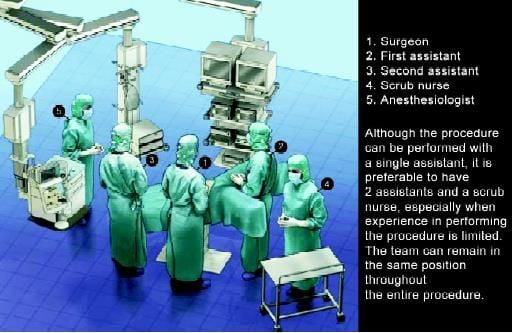
Position of a surgical team in colorectal surgery
Cannula Positioning
Standardize cannula placement is five or six cannulae for left-sided colectomies. This allows us to achieve excellent exposure which may be particularly valuable at the beginning of a surgeon's learning curve. Using six cannulae allows the use of more instruments in the abdominal cavity for retraction of bowel and structures especially in the presence of abundant intra-abdominal fat or of the dilated small bowel, as well as during mobilization of the splenic flexure.
Cannula fixation to the abdominal wall is important, to avoid CO2 leakage, and in cases of malignancy, to minimize the passage of tumor cells and help reduce the incidence of port-site metastases. This is mainly achieved by fitting the size of the incision to the cannula size or by fixing the cannula to the abdomen with a suture placed around the stopcock of the cannula. The use of screw-like cannulae has drawbacks that it increases the parietal trauma. Generally, it is better to perform an "open" technique for the insertion of the first cannula, which is placed at the midline, above the umbilicus, to reduce the risk of injury of abdominal organs. With some experience, the task becomes easy and very rapid. However, in the case of previous abdominal surgery, we usually inflate the abdominal cavity using the Veress needle in the left subcostal area, in order to insert the first cannula as far lateral as possible, in the right hypochondrium, to avoid potential areas of adhesions.
The first cannula (12 mm), which is used for the optical device, is positioned on the midline 3–4 cm above the umbilicus. The two operating cannulae are introduced, one at the junction between the umbilical line and the right midclavicular line, and the other 8–10 cm inferiorly, on the same line. The latter is a 12 mm operating cannula to allow the introduction of a linear stapler at the time of bowel resection. This cannula accommodates the following: scissors (monopolar, high-frequency hemostasis device, clip, staplers), a monopolar hook, surgical loops, a suction- irrigation device, and an atraumatic grasper. A fourth cannula is placed on the left midclavicular line, at the level of the umbilicus. This is a 5 mm cannula, which accommodates an atraumatic grasper used for retraction and exposure during the medial approach for the dissection of the left mesocolon. When performing mobilization of the splenic flexure, this cannula becomes an operating cannula. A fifth 5 mm cannula is placed 8–10 cm above the pubic bone, on the midline, and is used for retraction.
For most of the procedure, it accommodates a grasper used to expose the sigmoid and descending mesocolon. At the end of the procedure, the incision at this cannula's site is lengthened to allow the extraction of the specimen. Some surgeons sometimes use an additional cannula, which is a 5 mm cannula situated on the right midclavicular line in the subcostal area and accommodates an atraumatic grasper used to retract the terminal portion of the small intestine laterally at the beginning of the dissection and to retract the transverse colon during the mobilization of the splenic flexure.
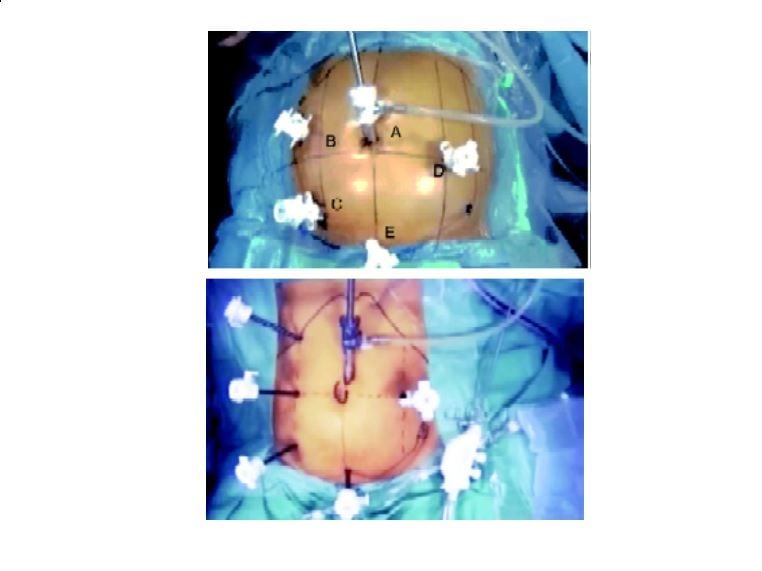
(A) Port position for sigmoidectomy for benign disease. (B) Alternating post position for sigmoidectomy for malignant disease.
Operative Technique
Exposure
To complete exposure of the operative field, active positioning of the bowel is usually necessary for addition to the passive action of gravity, especially in the presence of obesity or bowel dilatation. The greater omentum and the transverse colon are placed in the left subphrenic region and maintained in this position by the Trendelenburg tilt. An atraumatic retractor, introduced through the cannula on the left side, may also be used. Subsequently, the proximal small bowel loops are placed in the right upper quadrant using gentle grasping.
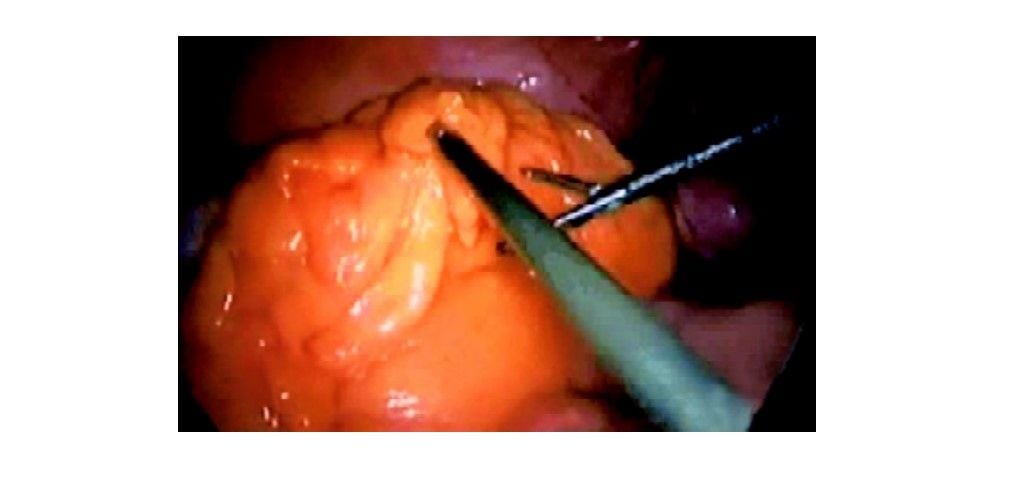
Exposure of sigmoid colon after shifting the omentum upward
The distal small bowel loops are placed in the right lower quadrant with the cecum and maintained there with gravity. If gravity is not sufficient, as occurs especially in the presence of abundant intraabdominal fat or dilated bowel, an additional maneuver is used. An instrument passed through the right subcostal cannula is passed at the root of the mesentery and grasps the parietal peritoneum of the right iliac fossa; the shaft of the grasper thus provides an auto-static retraction of the bowel loops, keeping them away from the midline and from the pelvic space. This technique of exposure provides an excellent view of the sacral promontory and of the aortoiliac axis. This particular view on the operative field is essential for the medial to lateral vascular approach.
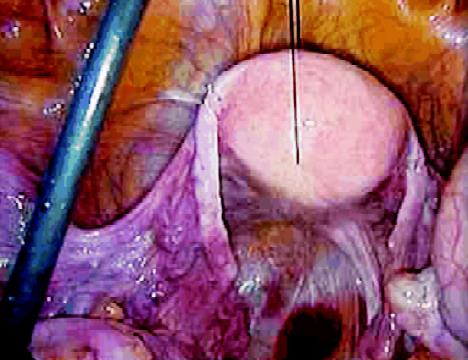
Securing the uterus by suture for proper exposure of rectum
The uterus may be an obstacle to adequate exposure in the pelvis. In postmenopausal women, the uterus can be suspended to the abdominal wall by a suture. This suture is introduced halfway between the umbilicus and the pubis and opens the rectovaginal space. In younger women, the uterus can be retracted using a similar suspension by a suture around the round ligaments or using a 5 mm retractor passed through the suprapubic cannula. Very often, conversion to open surgery is caused by difficulty in exposure, not only at the beginning but also throughout the procedure. To perform a medial approach, time is dedicated to the perfect achievement of this exposure, which will serve not only for the initial vascular approach but also for about half of the remaining operative time. After adequate exposure has been achieved, the following steps of the technique include the vascular approach, the medial posterior mobilization of the sigmoid, the extraction of the specimen, and the anastomosis. Additional steps include the mobilization of the splenic flexure, performed when further lengthening of the bowel is needed to perform a tension-free anastomosis. The step of the exposure is preliminary, and it is done in a similar manner, regardless of the type of disease. The remainder of the procedure is different if the indication for surgery is cancer or benign disease.
Sigmoid Colon Resection for Cancer
In laparoscopic colorectal sigmoidectomy for cancer or for benign disease, the vascular approach is the first step of the dissection. It is believed that it allows us to avoid unnecessary manipulation of the colon and tumor, which may cause tumor cell exfoliation, and to perform a good lymphadenectomy following the vascular anatomy. The vessels are gradually exposed once the peritoneum at the base of the sigmoid mesocolon is incised. The medial to lateral view allows us to see the sympathetic nerve plexus trunks, the left ureter, and gonadal vessels, avoiding ureteral injuries and possibly preserving genital function.
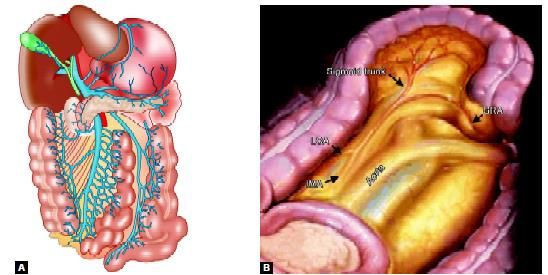
Vascular supply of left side of the colon
Primary Vascular Approach (Medial Approach)
Peritoneal Incision
The sigmoid mesocolon is retracted anteriorly, using a grasper introduced through the suprapubic cannula: This exposes the base of the sigmoid mesocolon. The visceral peritoneum is incised at the level of the sacral promontory. The incision is continued upward along the right anterior border of the aorta up to the ligament of Treitz. The pressure of the pneumoperitoneum facilitates the dissection, as the diffusion of CO2 opens the avascular planes.
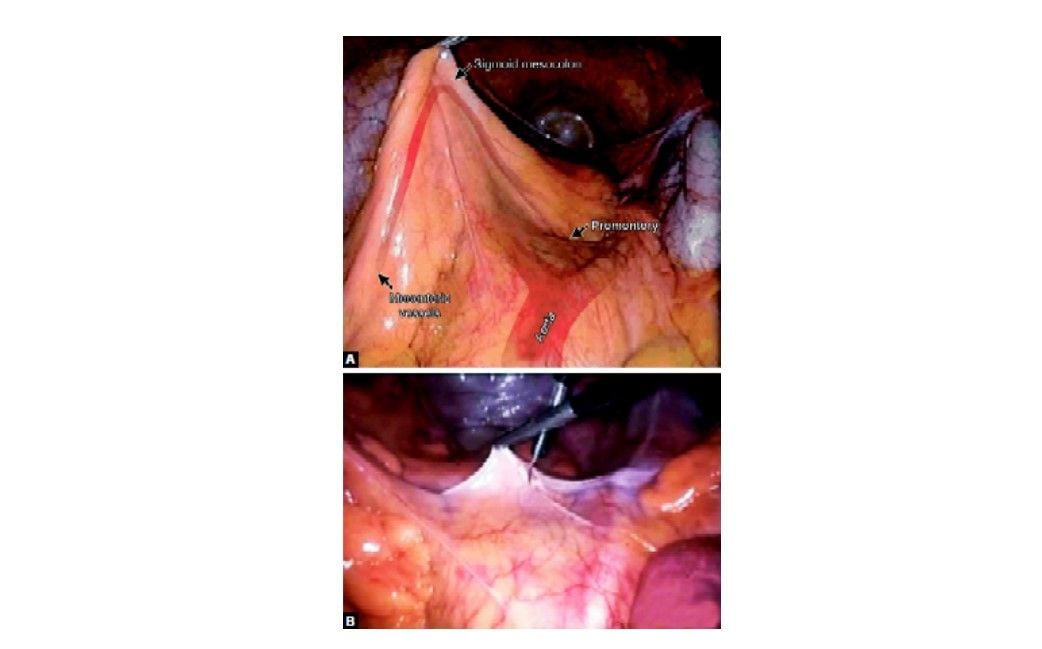
Incision of peritoneum over sacral promontory
Identification of the Inferior Mesenteric Artery
The dissection of the cellular adipose tissue is continued upward by gradually dividing the sigmoid branches of the right sympathetic trunk. The dissection behind the inferior mesenteric artery involves the preservation of the main hypogastric nerve trunks, but also the division of the small branches traveling to the colon to expose the origin of the inferior mesenteric artery. To ensure an adequate lymphadenectomy, the first 2 cm of the inferior mesenteric artery is dissected free and the artery is skeletonized before it is divided.
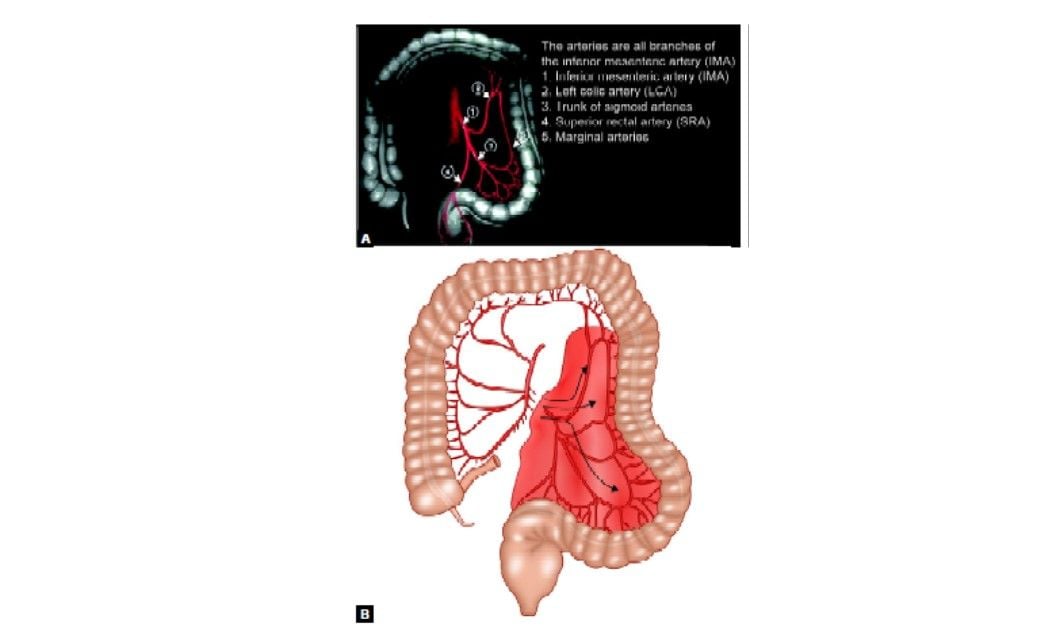
Arterial supply of sigmoid colon
This dissection at the origin of the inferior mesenteric artery involves a risk of injury to the left sympathetic trunk situated on the left border of the inferior mesenteric artery. A meticulous dissection of the artery (skeletonization) helps to avoid this risk, because only the vessel will be divided, and not the surrounding tissues. Dissection performed close to the artery also minimizes the risk of ureteral injury during the ligation of the inferior mesenteric artery. The inferior mesenteric artery can then be divided between clips, or by using a linear stapler (vascular 2.5 or 2.0 mm cartridges. The artery is divided at 1 to 2 cm distal to its origin from the aorta ideally after the take-off of the left colic artery.
Identification of the Inferior Mesenteric Vein
The inferior mesenteric vein (IMV) terminates when reaching the splenic vein, which goes on to form the portal vein with the superior mesenteric vein (SMV). Anatomical variations include the IMV draining into the confluence of the SMV and splenic vein and the IMV draining in the SMV. The inferior mesenteric vein (IMV) is identified to the left of the IMA or in case of difficulty, higher, just to the left of the ligament of Treitz junction. The vein is divided below the inferior border of the pancreas or above the left colic vein. Once again, clips are sure options to ligate and divide this vessel.
Mobilization of the Sigmoid and Descending Colon
The mobilization of the sigmoid colon follows the division of the vessels. This step includes the freeing of posterior and lateral attachments of the sigmoid colon and mesocolon and the division of the rectal and sigmoid mesenteries. The approach is either medial or lateral. It is wise to routinely perform this medial-to-lateral laparoscopic dissection for all indications. The medial approach is well adapted for laparoscopy because it preserves the working space and demands the least handling of the sigmoid colon. In a randomized trial comparing the medial-to-lateral laparoscopic dissection with the classical lateral-to-medial approach for resection of rectosigmoid cancer, Liang et al showed that the medial approach reduces operative time and the postoperative proinflammatory response. Besides the potential oncologic advantages of early vessel division and "no-touch" dissection, it is believed that the longer the lateral abdominal wall attachments of the colon are preserved, the easier are the exposure and dissection.
Posterior Detachment
The sigmoid mesocolon is retracted anteriorly using the suprapubic cannula to expose the posterior space. The plane between Toldt's fascia and the sigmoid mesocolon can then be identified. This plane is avascular and easily divided. The dissection continues posteriorly to the sigmoid mesocolon going laterally toward Toldt's line. The sigmoid colon is then completely free, and the lateral attachments can then be divided using a lateral approach.
Lateral Mobilization
The extent of the dissection is superiorly for the inferior border of the pancreas, laterally following Gerota's fascia and inferiorly for the psoas muscle where the ureter crosses the iliac vessels. The sigmoid loop is pulled toward the right upper quadrant (grasper in right subcostal cannula) to exert traction on the line of Toldt. The peritoneal fold is opened cephalad and caudad, and the dissection joins the one previously performed medially. During this step, care must be taken to avoid the gonadal vessels and the left ureter because they can be attracted by the traction exerted on the mesentery. Ureteral stenting (infrared stents) can be useful in cases in which inflammation, tumoral tissue, or adhesions and endometriosis make planes difficult to recognize.
Dissection of the Upper Mesorectum
This area of dissection should be approached with caution, especially on the left side: The mesorectum there is closely attached to the parietal fascia where the superior hypogastric nerve and the left ureter are situated. The upper portion of the rectum is mobilized posteriorly following the avascular plane described before, then laterally, until a sufficient distal margin is achieved.
Resection of the Specimen
Division of the Rectum
Once the upper rectum is freed, the area of distal resection is chosen, allowing a distal margin of at least 5 cm. The fat surrounding this area is cleared, using monopolar cautery, ultrasonic dissection, or the LigaSure device. In doing so, the superior hemorrhoidal arteries are divided into the posterior upper mesorectum. The distal division is performed using a linear stapler.
The stapler is introduced through the right lower quadrant cannula. It is wise to use stapler loads 3.5 mm, 45 mm blue cartridges, which are applied perpendicular to the bowel. Articulated staplers can also be useful, although they are usually unnecessary at the level of the upper rectum.
Proximal Division
The proximal division site should be located at least 10 cm proximal to the tumor. It is performed by first dividing the mesocolon and subsequently the bowel. The division of the mesocolon is more easily performed with the harmonic scalpel, or the LigaSure, although linear staplers can also be used. The distal portion of the divided IMA is identified, and the division of the mesocolon starts right at this level and continues toward the chosen proximal section site at a 90° angle. A linear stapler is then fired across the bowel. The stapler (blue load) is introduced through the right lower quadrant cannula. The specimen is placed in a plastic retrieval sac introduced through the same cannula. This permits the continuation of the procedure without manipulation of the bowel and tumor. If the resected specimen is large and obscures the operative fields, the extraction can be done before completing the mobilization of the left colon.
Mobilization of the Splenic Flexure
In the frequent event that a long segment of the sigmoid colon has been resected, mobilization of the splenic flexure is required. This can be achieved in different ways. It is important for the surgeon to be familiar with all approaches in order to select the most suitable approach. Sufficient mobilization of the splenic flexure may be achieved by simply freeing the posterior and lateral attachments of the descending colon. This is begun by a medial approach to free the posterior attachments of the descending and distal transverse colon, followed by the dissection of the lateral attachments, or by doing the same task in the reverse order. Lateral mobilization is sometimes sufficient in cases of sigmoid cancer, where the posterior mobilization can be omitted.
Lateral Mobilization of the Splenic Flexure
This approach is often used in open surgery and can also be used in simple laparoscopic colectomies. The first step is the section of the lateral attachments of the descending colon. An ascending incision is made along the line of Toldt using scissors introduced via the left-sided cannula. The phrenocolic ligament is then divided using scissors introduced through this cannula. Retraction of the descending colon and the splenic flexure toward the right lower quadrant using graspers introduced through the right lower and suprapubic cannulae helps to expose the correct plane. The attachments between the transverse colon and the omentum are divided close to the colon until the lesser sac is opened. The division of these attachments is continued as needed, to facilitate the mobilization of the colon into the pelvis.
Medial Mobilization
This approach dissects the posterior attachments of the transverse and descending colon first. The dissection plane naturally follows the plane of the previous sigmoid colon mobilization, cephalad, and anterior to Toldt's fascia. The transverse colon is retracted anteriorly to expose the inferior border of the pancreas, and the root of the transverse mesocolon is divided anterior to the pancreas and at a distance from it; to enter the lesser sac. The dissection then follows toward the base of the descending colon and distal transverse colon, dividing the posterior attachments of these structures. The division of the lateral attachments, as described above, then follows the full mobilization of the splenic flexure. If the mobilized colon reaches the pelvis easily, it may be safely assumed the anastomosis will be tension free as well.
Extraction of Colon
The extraction of the specimen is performed using double protection: A wound protector as well as a retrieval sac. The wound protector is also helpful to ensure that there is no CO2 leak during the intracorporeal colorectal anastomosis, which follows the extraction. This allows a reduction of the size of the incision and potentially minimizes the risk of tumor cell seeding.
The incision to Extract the Specimen
The size of the incision, its location, and the extraction technique take into account the volume of the specimen, the patient's body habitus, cosmetic concerns, and the type of disease. The incision is generally performed in the suprapubic region. The proximal division is performed intracorporeally, as described above, and the specimen placed into a thick plastic bag before being extracted through the incision at the suprapubic area.
Anastomosis
For anastomosis, a mechanical circular stapling device passed transanally to perform the anastomosis. Performing the anastomosis includes an extra-abdominal preparatory step and an intra-abdominal step performed laparoscopically. The extra-abdominal step takes place after the extraction of the specimen. The instrument holding the proximal bowel presents it at the incision where it can easily be grasped with a Babcock clamp and pulled out. If necessary, the colon is divided again in a healthy and well-vascularized zone. The anvil (at least 28 mm in diameter) is then introduced into the bowel lumen and closed with a purse-string; then the colon is reintroduced into the abdominal cavity. The abdominal incision is closed to re-establish the pneumoperitoneum. For an air-tight closure, it is sufficient to twist the wound protector at the level of the incision using a large clamp. The circular stapler is introduced into the rectum through the gently dilated anus. The rectal stump is then transfixed with the tip of the head of the circular stapler. In women, the posterior vaginal wall should be retracted anteriorly by the assistant passing the stapler. Once the center rod and anvil are clicked into the distal part of the circular stapler should be checked for twisting of the colon and the mesentery. The stapler is then fired after ensuring that the neighboring organs are away from the stapling line. The stapler is then twisted open and withdrawn. The anastomosis is checked for leaks by verifying the integrity of the proximal and distal rings, as well as performing an air test.
Wound Closure
The cannula sites are checked internally for possible hemorrhage. To do so, a grasper is passed through the cannula and the cannula is removed leaving the grasper in the abdomen. Because of the smaller diameter of the grasper compared with the cannula, if the bleeding was so far concealed by the tamponade effect of the cannula, it would be revealed promptly. The cannula is then reintroduced to allow maintenance of the pneumoperitoneum while performing the same check at all cannula sites.
When the check is completed, the CO2 is desufflated through the cannulae, and cannulae are removed. No routine drainage of the anastomotic area is performed. The suprapubic incision is closed in layers using running absorbable sutures, and all fascial defects of 10 mm and more are closed. The skin is closed with a subcuticular absorbable suture.
Laparoscopic sigmoid colon resection is indicated for both benign (diverticulitis, segmental Crohn's disease, polyp unresectable by colonoscopy) and malignant (primary colon cancer) etiologies, and is one of the most common operations done by laparoscopic methods. In chronic diverticular disease, the indications for laparoscopic sigmoid resection are the same as for open surgery. Sigmoid colectomy for diverticulitis can be technically challenging because of severe inflammation in the left-lower quadrant and pelvis.
Patient Positioning and Operating Room Setup
A proper patient position is key to both facilitating operative maneuvers and preventing complications such as nerve and vein compression, and traction injuries to the brachial plexus. The patient is placed supine, in the modified lithotomy position, with legs abducted and slightly flexed at the knees. The patient's right arm is alongside the body, whereas the left arm is usually placed at a 90° angle. Adequate padding is used to avoid compression on bone prominences. A nasogastric or orogastric tube and a urinary catheter are placed. Adequate thromboembolism prophylaxis should be used, as preferred by the surgeon, and intermittent leg compression stockings can be used as well. The procedure is usually performed with two assistants and a scrub nurse. The surgeon is on the right side of the patient and the second assistant is also on the right side. The first assistant stands between the patient's legs and the scrub nurse at the lower right side of the table. The team remains in the same position throughout the entire procedure. It is advisable to use a table that can be easily tilted laterally and placed into steep Trendelenburg and reverse Trendelenburg position, in order to facilitate exposure of the pelvic space and of the splenic flexure. The laparoscopic unit with the main monitor is located on the left side of the table. It is useful to use a second monitor placed above the patient's head.
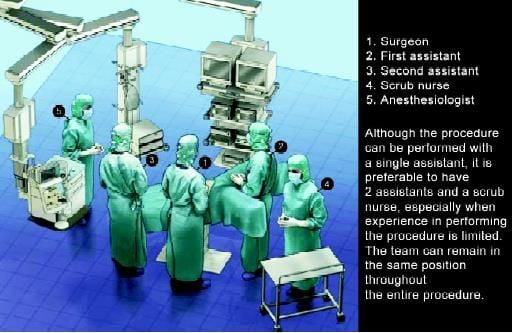
Position of a surgical team in colorectal surgery
Cannula Positioning
Standardize cannula placement is five or six cannulae for left-sided colectomies. This allows us to achieve excellent exposure which may be particularly valuable at the beginning of a surgeon's learning curve. Using six cannulae allows the use of more instruments in the abdominal cavity for retraction of bowel and structures especially in the presence of abundant intra-abdominal fat or of the dilated small bowel, as well as during mobilization of the splenic flexure.
Cannula fixation to the abdominal wall is important, to avoid CO2 leakage, and in cases of malignancy, to minimize the passage of tumor cells and help reduce the incidence of port-site metastases. This is mainly achieved by fitting the size of the incision to the cannula size or by fixing the cannula to the abdomen with a suture placed around the stopcock of the cannula. The use of screw-like cannulae has drawbacks that it increases the parietal trauma. Generally, it is better to perform an "open" technique for the insertion of the first cannula, which is placed at the midline, above the umbilicus, to reduce the risk of injury of abdominal organs. With some experience, the task becomes easy and very rapid. However, in the case of previous abdominal surgery, we usually inflate the abdominal cavity using the Veress needle in the left subcostal area, in order to insert the first cannula as far lateral as possible, in the right hypochondrium, to avoid potential areas of adhesions.
The first cannula (12 mm), which is used for the optical device, is positioned on the midline 3–4 cm above the umbilicus. The two operating cannulae are introduced, one at the junction between the umbilical line and the right midclavicular line, and the other 8–10 cm inferiorly, on the same line. The latter is a 12 mm operating cannula to allow the introduction of a linear stapler at the time of bowel resection. This cannula accommodates the following: scissors (monopolar, high-frequency hemostasis device, clip, staplers), a monopolar hook, surgical loops, a suction- irrigation device, and an atraumatic grasper. A fourth cannula is placed on the left midclavicular line, at the level of the umbilicus. This is a 5 mm cannula, which accommodates an atraumatic grasper used for retraction and exposure during the medial approach for the dissection of the left mesocolon. When performing mobilization of the splenic flexure, this cannula becomes an operating cannula. A fifth 5 mm cannula is placed 8–10 cm above the pubic bone, on the midline, and is used for retraction.
For most of the procedure, it accommodates a grasper used to expose the sigmoid and descending mesocolon. At the end of the procedure, the incision at this cannula's site is lengthened to allow the extraction of the specimen. Some surgeons sometimes use an additional cannula, which is a 5 mm cannula situated on the right midclavicular line in the subcostal area and accommodates an atraumatic grasper used to retract the terminal portion of the small intestine laterally at the beginning of the dissection and to retract the transverse colon during the mobilization of the splenic flexure.
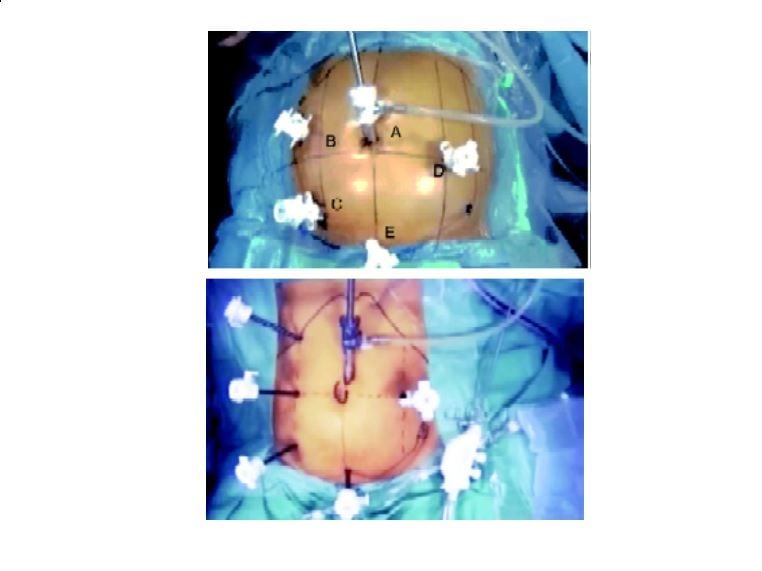
(A) Port position for sigmoidectomy for benign disease. (B) Alternating post position for sigmoidectomy for malignant disease.
Operative Technique
Exposure
To complete exposure of the operative field, active positioning of the bowel is usually necessary for addition to the passive action of gravity, especially in the presence of obesity or bowel dilatation. The greater omentum and the transverse colon are placed in the left subphrenic region and maintained in this position by the Trendelenburg tilt. An atraumatic retractor, introduced through the cannula on the left side, may also be used. Subsequently, the proximal small bowel loops are placed in the right upper quadrant using gentle grasping.
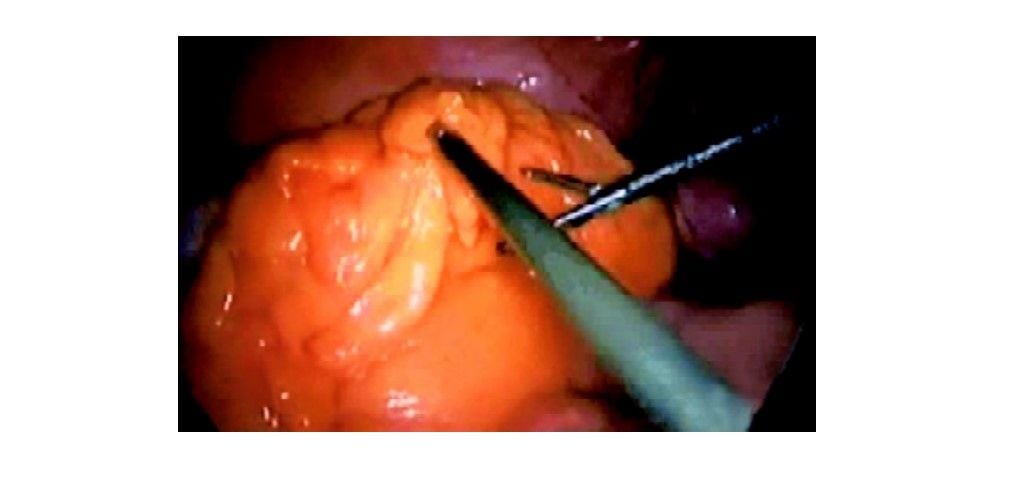
Exposure of sigmoid colon after shifting the omentum upward
The distal small bowel loops are placed in the right lower quadrant with the cecum and maintained there with gravity. If gravity is not sufficient, as occurs especially in the presence of abundant intraabdominal fat or dilated bowel, an additional maneuver is used. An instrument passed through the right subcostal cannula is passed at the root of the mesentery and grasps the parietal peritoneum of the right iliac fossa; the shaft of the grasper thus provides an auto-static retraction of the bowel loops, keeping them away from the midline and from the pelvic space. This technique of exposure provides an excellent view of the sacral promontory and of the aortoiliac axis. This particular view on the operative field is essential for the medial to lateral vascular approach.
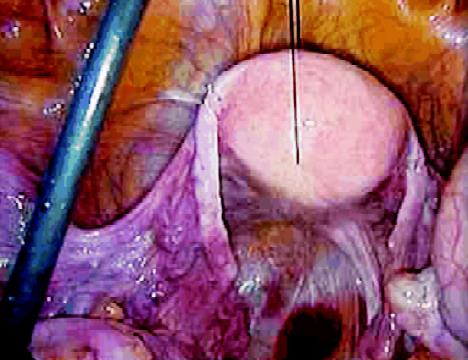
Securing the uterus by suture for proper exposure of rectum
The uterus may be an obstacle to adequate exposure in the pelvis. In postmenopausal women, the uterus can be suspended to the abdominal wall by a suture. This suture is introduced halfway between the umbilicus and the pubis and opens the rectovaginal space. In younger women, the uterus can be retracted using a similar suspension by a suture around the round ligaments or using a 5 mm retractor passed through the suprapubic cannula. Very often, conversion to open surgery is caused by difficulty in exposure, not only at the beginning but also throughout the procedure. To perform a medial approach, time is dedicated to the perfect achievement of this exposure, which will serve not only for the initial vascular approach but also for about half of the remaining operative time. After adequate exposure has been achieved, the following steps of the technique include the vascular approach, the medial posterior mobilization of the sigmoid, the extraction of the specimen, and the anastomosis. Additional steps include the mobilization of the splenic flexure, performed when further lengthening of the bowel is needed to perform a tension-free anastomosis. The step of the exposure is preliminary, and it is done in a similar manner, regardless of the type of disease. The remainder of the procedure is different if the indication for surgery is cancer or benign disease.
Sigmoid Colon Resection for Cancer
In laparoscopic colorectal sigmoidectomy for cancer or for benign disease, the vascular approach is the first step of the dissection. It is believed that it allows us to avoid unnecessary manipulation of the colon and tumor, which may cause tumor cell exfoliation, and to perform a good lymphadenectomy following the vascular anatomy. The vessels are gradually exposed once the peritoneum at the base of the sigmoid mesocolon is incised. The medial to lateral view allows us to see the sympathetic nerve plexus trunks, the left ureter, and gonadal vessels, avoiding ureteral injuries and possibly preserving genital function.
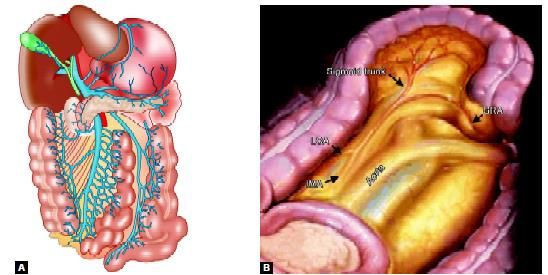
Vascular supply of left side of the colon
Primary Vascular Approach (Medial Approach)
Peritoneal Incision
The sigmoid mesocolon is retracted anteriorly, using a grasper introduced through the suprapubic cannula: This exposes the base of the sigmoid mesocolon. The visceral peritoneum is incised at the level of the sacral promontory. The incision is continued upward along the right anterior border of the aorta up to the ligament of Treitz. The pressure of the pneumoperitoneum facilitates the dissection, as the diffusion of CO2 opens the avascular planes.
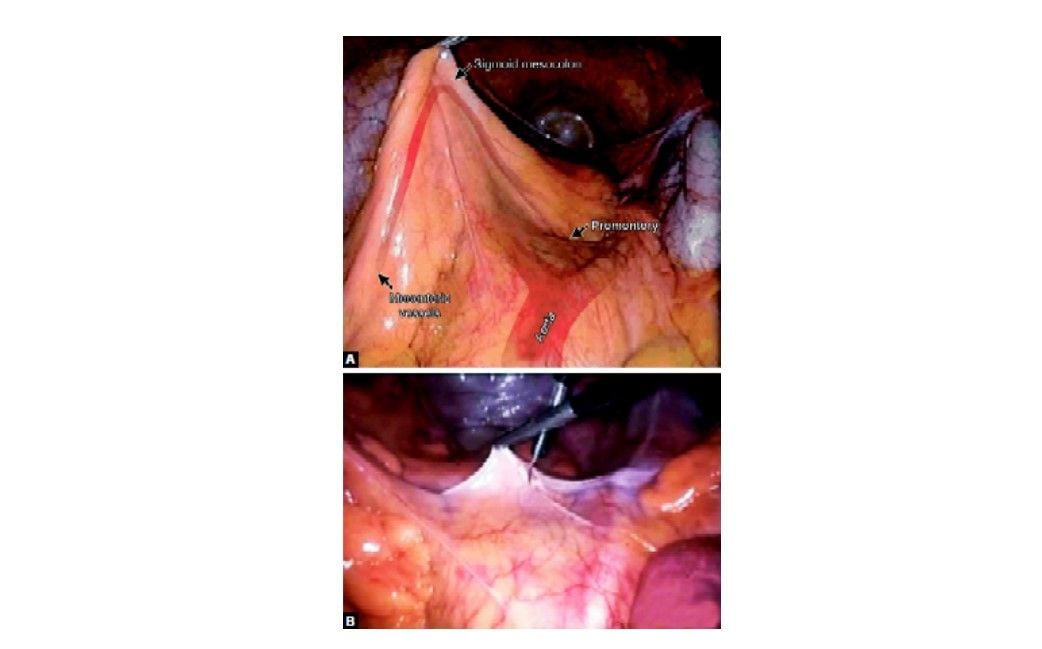
Incision of peritoneum over sacral promontory
Identification of the Inferior Mesenteric Artery
The dissection of the cellular adipose tissue is continued upward by gradually dividing the sigmoid branches of the right sympathetic trunk. The dissection behind the inferior mesenteric artery involves the preservation of the main hypogastric nerve trunks, but also the division of the small branches traveling to the colon to expose the origin of the inferior mesenteric artery. To ensure an adequate lymphadenectomy, the first 2 cm of the inferior mesenteric artery is dissected free and the artery is skeletonized before it is divided.
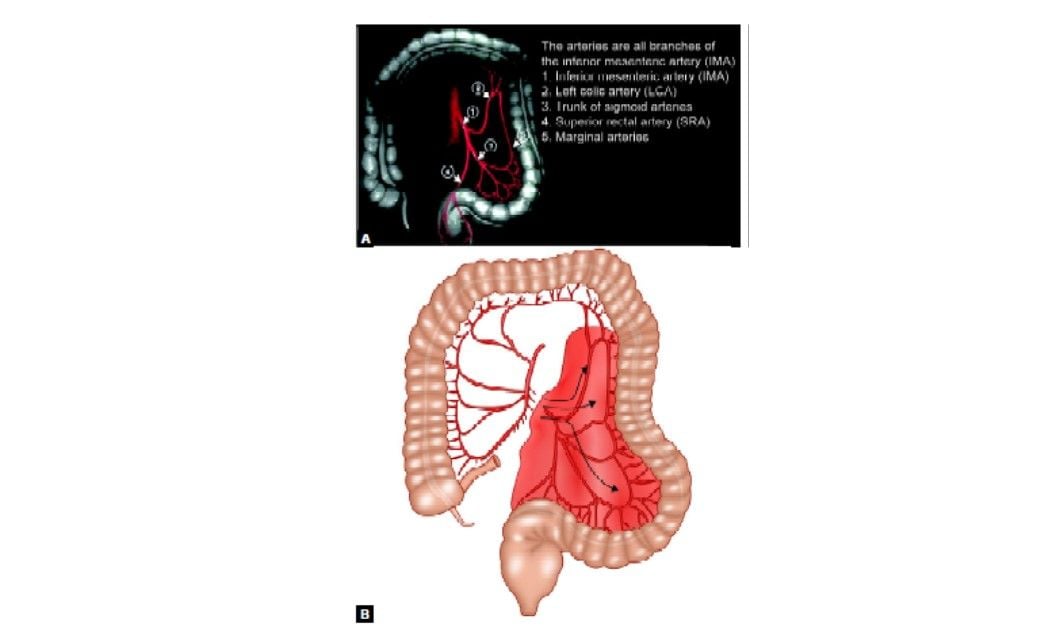
Arterial supply of sigmoid colon
This dissection at the origin of the inferior mesenteric artery involves a risk of injury to the left sympathetic trunk situated on the left border of the inferior mesenteric artery. A meticulous dissection of the artery (skeletonization) helps to avoid this risk, because only the vessel will be divided, and not the surrounding tissues. Dissection performed close to the artery also minimizes the risk of ureteral injury during the ligation of the inferior mesenteric artery. The inferior mesenteric artery can then be divided between clips, or by using a linear stapler (vascular 2.5 or 2.0 mm cartridges. The artery is divided at 1 to 2 cm distal to its origin from the aorta ideally after the take-off of the left colic artery.
Identification of the Inferior Mesenteric Vein
The inferior mesenteric vein (IMV) terminates when reaching the splenic vein, which goes on to form the portal vein with the superior mesenteric vein (SMV). Anatomical variations include the IMV draining into the confluence of the SMV and splenic vein and the IMV draining in the SMV. The inferior mesenteric vein (IMV) is identified to the left of the IMA or in case of difficulty, higher, just to the left of the ligament of Treitz junction. The vein is divided below the inferior border of the pancreas or above the left colic vein. Once again, clips are sure options to ligate and divide this vessel.
Mobilization of the Sigmoid and Descending Colon
The mobilization of the sigmoid colon follows the division of the vessels. This step includes the freeing of posterior and lateral attachments of the sigmoid colon and mesocolon and the division of the rectal and sigmoid mesenteries. The approach is either medial or lateral. It is wise to routinely perform this medial-to-lateral laparoscopic dissection for all indications. The medial approach is well adapted for laparoscopy because it preserves the working space and demands the least handling of the sigmoid colon. In a randomized trial comparing the medial-to-lateral laparoscopic dissection with the classical lateral-to-medial approach for resection of rectosigmoid cancer, Liang et al showed that the medial approach reduces operative time and the postoperative proinflammatory response. Besides the potential oncologic advantages of early vessel division and "no-touch" dissection, it is believed that the longer the lateral abdominal wall attachments of the colon are preserved, the easier are the exposure and dissection.
Posterior Detachment
The sigmoid mesocolon is retracted anteriorly using the suprapubic cannula to expose the posterior space. The plane between Toldt's fascia and the sigmoid mesocolon can then be identified. This plane is avascular and easily divided. The dissection continues posteriorly to the sigmoid mesocolon going laterally toward Toldt's line. The sigmoid colon is then completely free, and the lateral attachments can then be divided using a lateral approach.
Lateral Mobilization
The extent of the dissection is superiorly for the inferior border of the pancreas, laterally following Gerota's fascia and inferiorly for the psoas muscle where the ureter crosses the iliac vessels. The sigmoid loop is pulled toward the right upper quadrant (grasper in right subcostal cannula) to exert traction on the line of Toldt. The peritoneal fold is opened cephalad and caudad, and the dissection joins the one previously performed medially. During this step, care must be taken to avoid the gonadal vessels and the left ureter because they can be attracted by the traction exerted on the mesentery. Ureteral stenting (infrared stents) can be useful in cases in which inflammation, tumoral tissue, or adhesions and endometriosis make planes difficult to recognize.
Dissection of the Upper Mesorectum
This area of dissection should be approached with caution, especially on the left side: The mesorectum there is closely attached to the parietal fascia where the superior hypogastric nerve and the left ureter are situated. The upper portion of the rectum is mobilized posteriorly following the avascular plane described before, then laterally, until a sufficient distal margin is achieved.
Resection of the Specimen
Division of the Rectum
Once the upper rectum is freed, the area of distal resection is chosen, allowing a distal margin of at least 5 cm. The fat surrounding this area is cleared, using monopolar cautery, ultrasonic dissection, or the LigaSure device. In doing so, the superior hemorrhoidal arteries are divided into the posterior upper mesorectum. The distal division is performed using a linear stapler.
The stapler is introduced through the right lower quadrant cannula. It is wise to use stapler loads 3.5 mm, 45 mm blue cartridges, which are applied perpendicular to the bowel. Articulated staplers can also be useful, although they are usually unnecessary at the level of the upper rectum.
Proximal Division
The proximal division site should be located at least 10 cm proximal to the tumor. It is performed by first dividing the mesocolon and subsequently the bowel. The division of the mesocolon is more easily performed with the harmonic scalpel, or the LigaSure, although linear staplers can also be used. The distal portion of the divided IMA is identified, and the division of the mesocolon starts right at this level and continues toward the chosen proximal section site at a 90° angle. A linear stapler is then fired across the bowel. The stapler (blue load) is introduced through the right lower quadrant cannula. The specimen is placed in a plastic retrieval sac introduced through the same cannula. This permits the continuation of the procedure without manipulation of the bowel and tumor. If the resected specimen is large and obscures the operative fields, the extraction can be done before completing the mobilization of the left colon.
Mobilization of the Splenic Flexure
In the frequent event that a long segment of the sigmoid colon has been resected, mobilization of the splenic flexure is required. This can be achieved in different ways. It is important for the surgeon to be familiar with all approaches in order to select the most suitable approach. Sufficient mobilization of the splenic flexure may be achieved by simply freeing the posterior and lateral attachments of the descending colon. This is begun by a medial approach to free the posterior attachments of the descending and distal transverse colon, followed by the dissection of the lateral attachments, or by doing the same task in the reverse order. Lateral mobilization is sometimes sufficient in cases of sigmoid cancer, where the posterior mobilization can be omitted.
Lateral Mobilization of the Splenic Flexure
This approach is often used in open surgery and can also be used in simple laparoscopic colectomies. The first step is the section of the lateral attachments of the descending colon. An ascending incision is made along the line of Toldt using scissors introduced via the left-sided cannula. The phrenocolic ligament is then divided using scissors introduced through this cannula. Retraction of the descending colon and the splenic flexure toward the right lower quadrant using graspers introduced through the right lower and suprapubic cannulae helps to expose the correct plane. The attachments between the transverse colon and the omentum are divided close to the colon until the lesser sac is opened. The division of these attachments is continued as needed, to facilitate the mobilization of the colon into the pelvis.
Medial Mobilization
This approach dissects the posterior attachments of the transverse and descending colon first. The dissection plane naturally follows the plane of the previous sigmoid colon mobilization, cephalad, and anterior to Toldt's fascia. The transverse colon is retracted anteriorly to expose the inferior border of the pancreas, and the root of the transverse mesocolon is divided anterior to the pancreas and at a distance from it; to enter the lesser sac. The dissection then follows toward the base of the descending colon and distal transverse colon, dividing the posterior attachments of these structures. The division of the lateral attachments, as described above, then follows the full mobilization of the splenic flexure. If the mobilized colon reaches the pelvis easily, it may be safely assumed the anastomosis will be tension free as well.
Extraction of Colon
The extraction of the specimen is performed using double protection: A wound protector as well as a retrieval sac. The wound protector is also helpful to ensure that there is no CO2 leak during the intracorporeal colorectal anastomosis, which follows the extraction. This allows a reduction of the size of the incision and potentially minimizes the risk of tumor cell seeding.
The incision to Extract the Specimen
The size of the incision, its location, and the extraction technique take into account the volume of the specimen, the patient's body habitus, cosmetic concerns, and the type of disease. The incision is generally performed in the suprapubic region. The proximal division is performed intracorporeally, as described above, and the specimen placed into a thick plastic bag before being extracted through the incision at the suprapubic area.
Anastomosis
For anastomosis, a mechanical circular stapling device passed transanally to perform the anastomosis. Performing the anastomosis includes an extra-abdominal preparatory step and an intra-abdominal step performed laparoscopically. The extra-abdominal step takes place after the extraction of the specimen. The instrument holding the proximal bowel presents it at the incision where it can easily be grasped with a Babcock clamp and pulled out. If necessary, the colon is divided again in a healthy and well-vascularized zone. The anvil (at least 28 mm in diameter) is then introduced into the bowel lumen and closed with a purse-string; then the colon is reintroduced into the abdominal cavity. The abdominal incision is closed to re-establish the pneumoperitoneum. For an air-tight closure, it is sufficient to twist the wound protector at the level of the incision using a large clamp. The circular stapler is introduced into the rectum through the gently dilated anus. The rectal stump is then transfixed with the tip of the head of the circular stapler. In women, the posterior vaginal wall should be retracted anteriorly by the assistant passing the stapler. Once the center rod and anvil are clicked into the distal part of the circular stapler should be checked for twisting of the colon and the mesentery. The stapler is then fired after ensuring that the neighboring organs are away from the stapling line. The stapler is then twisted open and withdrawn. The anastomosis is checked for leaks by verifying the integrity of the proximal and distal rings, as well as performing an air test.
Wound Closure
The cannula sites are checked internally for possible hemorrhage. To do so, a grasper is passed through the cannula and the cannula is removed leaving the grasper in the abdomen. Because of the smaller diameter of the grasper compared with the cannula, if the bleeding was so far concealed by the tamponade effect of the cannula, it would be revealed promptly. The cannula is then reintroduced to allow maintenance of the pneumoperitoneum while performing the same check at all cannula sites.
When the check is completed, the CO2 is desufflated through the cannulae, and cannulae are removed. No routine drainage of the anastomotic area is performed. The suprapubic incision is closed in layers using running absorbable sutures, and all fascial defects of 10 mm and more are closed. The skin is closed with a subcuticular absorbable suture.






