Laparoscopic Ovarian Surgery
Most ovarian abnormalities can be managed laparoscopically. The first laparoscopic salpingo-oophorectomy was performed by Semm in 1984. He reported his experience with a laparoscopic approach to oophorectomy and salpingo-oophorectomy. Laparoscopy may be an alternative of hysterectomy and more conservative management of pain caused by the adnexal disease can be performed. If necessary, oophorectomy can be performed laparoscopically with a short hospital stay and recovery period at a later date.
Laparoscopic Ovarian Anatomy
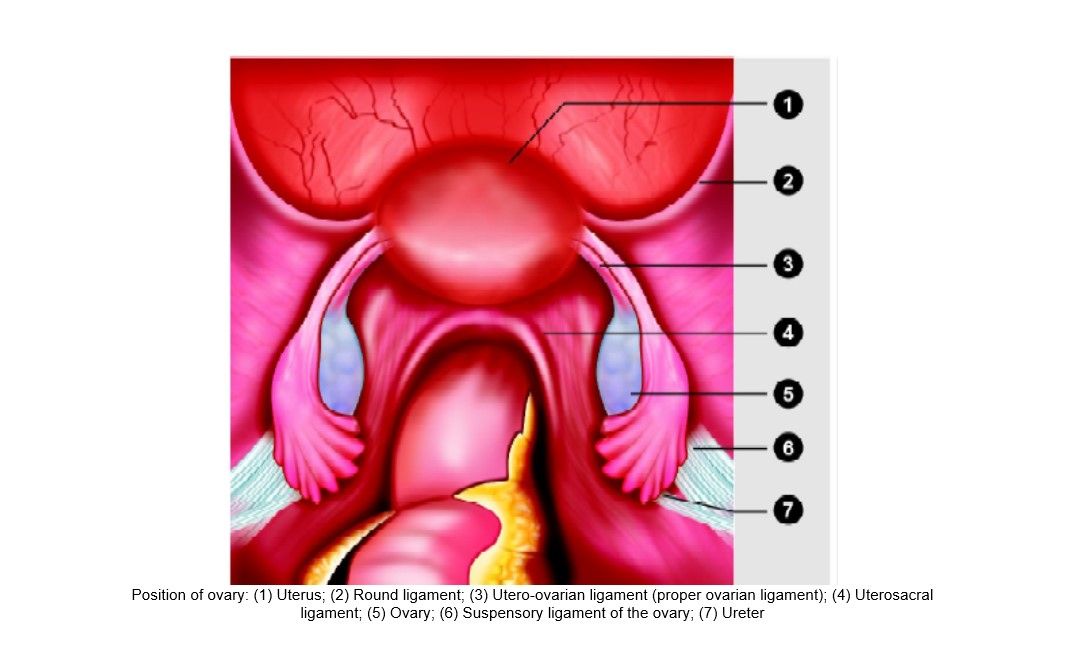
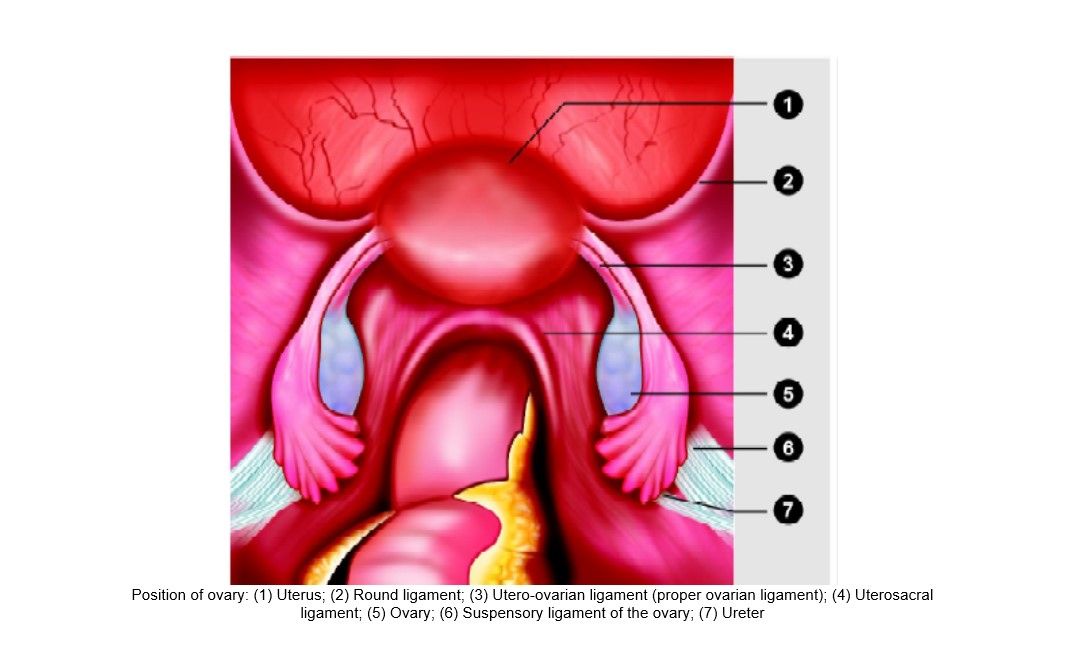
The ovaries are seen clearly by laparoscope because of their whiteness and knobby texture. It is seen more clearly if the uterine manipulator is used and the uterus is pushed towards the anterior abdominal wall. Ovaries hang down in the laparoscopic field. A normal ovary is almond-shaped, and approximately 3 cm in diameter. The ovarian ligaments run from the ovaries to the lateral border of the uterus. The ovary is attached to the pelvic sidewall with infundibulopelvic ligament, which carries the ovarian artery. One of the common mistakes is the injury of the ureter during dissection of the infundibulopelvic ligament. If the uterus deviates to the contralateral side with the help of uterine manipulator infundibulopelvic ligament is spread out and a pelvic sidewall triangle is created. The base of this triangle is the round ligament, the medial side is the infundibulopelvic ligament, and the lateral side is the external iliac artery. The apex of this triangle is the point at which the infundibulopelvic ligament crosses the external iliac artery. The ovarian arteries arise from the aorta to descend laterally to the ureter and genitofemoral nerve. The artery and accompanying vein cross over the external and internal iliac vessels to enter the pelvis. The left ovarian vein joins the left renal vein and the right ovarian vein joins the inferior vena cava.
Anatomy of the ovary
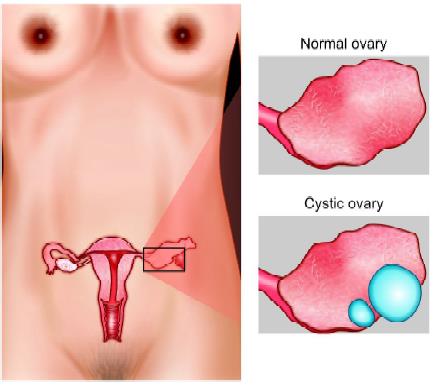
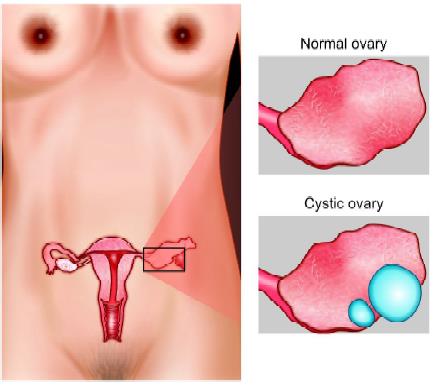
Laparoscopic Manage of Ovarian Cyst
Ovarian cysts are sacs filled with fluid or semisolid material that develops on or within the ovary. Surgery is indicated if the growth is larger than 4 inches (10 cm), complex, growing, persistent, solid, and irregularly shaped, on both ovaries, or causes pain or other symptoms. Laparoscopic management of ovarian cyst depends on the patient’s age, pelvic examination, sonographic images, and serum markers. A large, solid, fixed, or irregular adnexal mass accompanied by ascites is suspicious for malignancy. Cul-de-sac nodularity, ascites, cystic adnexal structures, and fixed adnexa occur with endometriosis and ovarian malignancy. Before selecting any case for laparoscopy, Ca- 125, an ovarian cancer marker, should be estimated, which may help to identify cancerous cysts in older women. Although ovarian neoplasms can occur at any age, the risk of malignancy is highest during prepuberty and menopause. Malignancy is not the only concern in managing an ovarian cyst. Patients who wish to preserve their reproductive organs should have the least aggressive therapy. In a postmenopausal patient whose family has a history of ovarian cancer, Ca-125 levels may help to detect it in the early stages. However, a surgeon should keep in mind that many benign gynecologic disorders are also associated with elevated Ca-125 levels, including fibroid uterus, endometriosis, and salpingitis that could lead to unnecessary concern and intervention. Because the risk of malignancy is relatively low in young women, preoperative evaluation should include a history and physical examination. Pelvic ultrasound should be performed to evaluate both ovaries to rule out bilateral endometriomas or teratoma. Hormone levels (such as LH, FSH, estradiol, and testosterone) may be checked to evaluate for associated hormonal conditions. The persistent ovarian cysts must be treated surgically, and evolving laparoscopic technology has enabled endoscopic management of most of them. Although most are benign, the possibility of malignancy usually requires a laparotomy using a midline incision. Oral contraceptives have been prescribed for some small cystic adnexal masses in reproductive-aged women on the assumption that decreasing gonadotropin stimulation to a functional cyst will hasten its resolution. Either danazol (800 mg/d) or oral contraceptive pills with 50 pg estrogen are advised for any cyst suspected of being functional. Crossing the true brim of the pelvis the following important tubular structures are found. The round ligament of the uterus, the infundibulopelvic ligament, which contains the gonadal vessels and the ureter. The ovaries and fallopian tube is found between the round ligament and the infundibulopelvic ligament.
Patient Position
The patient should be in steep Trendelenburg and lithotomy position. One assistant should remain between the legs of the patient to do uterine manipulation whenever required.
Port Position
The port position should be in accordance with the baseball diamond concept. If the cyst is of the right side, one port should be in the left iliac fossa and another in the right hypochondrium.
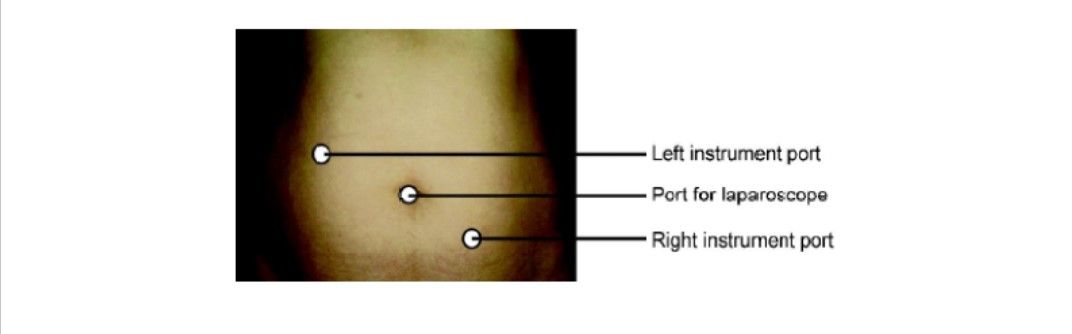
Port position for right-sided ovarian surgery
Operative Procedure
After access, the pelvis and upper abdomen have been examined, the cyst contents should be aspirated. Once the capsule is opened, the interior of the capsule is examined and suspicious areas should be sent for biopsy. The entire cyst capsule must be removed to search for an early carcinoma. Whether to perform oophorectomy or cystectomy depends on the patient’s age and characteristics of the mass.
Ovarian Cystectomy
Medical management of endometriomas has proven ineffective, either laparotomy or operative laparoscopy is necessary. Laparoscopic ovarian cystectomy removes the cyst with minimal trauma to the residual ovarian tissue. Laparotomy for ovarian cystectomy is not a good procedure because of the increased risk of ovarian adhesion formation. Three methods to manage such cysts are drainage, excision, and thermal coagulation. By excising the unruptured cyst, a histopathologic examination is more complete and the risk of recurrence is minimized, but laparoscopic removal of the intact cyst is very difficult and aspiration is recommended for functional cysts, which are diagnosed laparoscopically. Many cysts are ruptured during their manipulation despite a delicate technique.
Thermal ablation does not destroy the entire cyst wall, and the underlying ovarian cortex can be damaged by the heat. Therefore, the excision of the entire cyst wall with the help of blunt stripping and sharp dissection by scissors is recommended. The removal of a cyst 10 cm or larger is difficult laparoscopically. Aspiration before removal of large cysts is practical and can be accomplished using an 18 gauge needle passed through the separate puncture of the abdominal wall while stabilizing the cyst. The suction irrigation instrument can also be used to aspirate the content of the cyst. If gross characteristics of ovary look suspicious for malignancy. Some gynecologists recommend peritoneal washing before puncturing an ovarian cyst, because any cyst may be malignant. The peritoneal fluid or washings should be sent for cytological examination.
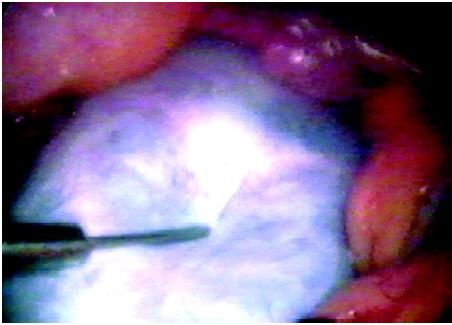
An ovarian cyst is aspirated for ovarian cystectomy
After the aspiration capsule of cyst is stripped from the ovarian stroma using two grasping forceps and the suction- irrigator probe for traction and counter traction. The electrosurgery can be used at low power to seal blood vessels at the base of the capsule and at higher powers to vaporize small remnants of a capsule. Bipolar forceps also can be used to control bleeding. The open jaw of bipolar can touch the oozing area and hemostasis can be achieved. Sometimes it is difficult to remove the capsule from the ovarian cortex so that injecting dilute vasopressin between the capsule and cortex facilitates the stripping procedure. If the cyst wall cannot be identified clearly, the edge of the ovarian incision can be “freshened” with scissors and the resulting clean edge reveals the two-layer, the outer layer will be ovarian and inner cystic. If this does not free the capsule, the base of the cyst is grasped, and traction applied to the cyst with counter traction to the ovary.
Sometimes the complete cyst or portions of the wall may be densely adherent to the ovary, requiring sharp or electrosurgical dissection to completely free the cyst wall. Generally, when the cyst capsule is removed from the ovary, the contraction of the ovarian capsule provides significant hemostasis. Bleeding can occur at the base, particularly if the cyst was close to the hilum. Under these circumstances, a needle electrode or a fine bipolar forceps can be used to minimize thermal damage. Large cysts sometimes need partial oophorectomy, to remove the distorted portion of the ovary, and the remaining cyst wall can be stripped from the ovarian stroma. Teratoma often can be excised intact but often the cyst rupture. After extraction, if the ovarian edges overlap itself, the defect is left to heal without suturing because adhesions are more likely, following the use of suture. In rare instances one or two fine, absorbable monofilament sutures may be needed to approximate the ovarian edges. The sutures are placed inside the ovary to decrease the formation of adhesions.
Most ovarian abnormalities can be managed laparoscopically. The first laparoscopic salpingo-oophorectomy was performed by Semm in 1984. He reported his experience with a laparoscopic approach to oophorectomy and salpingo-oophorectomy. Laparoscopy may be an alternative of hysterectomy and more conservative management of pain caused by the adnexal disease can be performed. If necessary, oophorectomy can be performed laparoscopically with a short hospital stay and recovery period at a later date.
Laparoscopic Ovarian Anatomy
The ovaries are seen clearly by laparoscope because of their whiteness and knobby texture. It is seen more clearly if the uterine manipulator is used and the uterus is pushed towards the anterior abdominal wall. Ovaries hang down in the laparoscopic field. A normal ovary is almond-shaped, and approximately 3 cm in diameter. The ovarian ligaments run from the ovaries to the lateral border of the uterus. The ovary is attached to the pelvic sidewall with infundibulopelvic ligament, which carries the ovarian artery. One of the common mistakes is the injury of the ureter during dissection of the infundibulopelvic ligament. If the uterus deviates to the contralateral side with the help of uterine manipulator infundibulopelvic ligament is spread out and a pelvic sidewall triangle is created. The base of this triangle is the round ligament, the medial side is the infundibulopelvic ligament, and the lateral side is the external iliac artery. The apex of this triangle is the point at which the infundibulopelvic ligament crosses the external iliac artery. The ovarian arteries arise from the aorta to descend laterally to the ureter and genitofemoral nerve. The artery and accompanying vein cross over the external and internal iliac vessels to enter the pelvis. The left ovarian vein joins the left renal vein and the right ovarian vein joins the inferior vena cava.
Anatomy of the ovary
Laparoscopic Manage of Ovarian Cyst
Ovarian cysts are sacs filled with fluid or semisolid material that develops on or within the ovary. Surgery is indicated if the growth is larger than 4 inches (10 cm), complex, growing, persistent, solid, and irregularly shaped, on both ovaries, or causes pain or other symptoms. Laparoscopic management of ovarian cyst depends on the patient’s age, pelvic examination, sonographic images, and serum markers. A large, solid, fixed, or irregular adnexal mass accompanied by ascites is suspicious for malignancy. Cul-de-sac nodularity, ascites, cystic adnexal structures, and fixed adnexa occur with endometriosis and ovarian malignancy. Before selecting any case for laparoscopy, Ca- 125, an ovarian cancer marker, should be estimated, which may help to identify cancerous cysts in older women. Although ovarian neoplasms can occur at any age, the risk of malignancy is highest during prepuberty and menopause. Malignancy is not the only concern in managing an ovarian cyst. Patients who wish to preserve their reproductive organs should have the least aggressive therapy. In a postmenopausal patient whose family has a history of ovarian cancer, Ca-125 levels may help to detect it in the early stages. However, a surgeon should keep in mind that many benign gynecologic disorders are also associated with elevated Ca-125 levels, including fibroid uterus, endometriosis, and salpingitis that could lead to unnecessary concern and intervention. Because the risk of malignancy is relatively low in young women, preoperative evaluation should include a history and physical examination. Pelvic ultrasound should be performed to evaluate both ovaries to rule out bilateral endometriomas or teratoma. Hormone levels (such as LH, FSH, estradiol, and testosterone) may be checked to evaluate for associated hormonal conditions. The persistent ovarian cysts must be treated surgically, and evolving laparoscopic technology has enabled endoscopic management of most of them. Although most are benign, the possibility of malignancy usually requires a laparotomy using a midline incision. Oral contraceptives have been prescribed for some small cystic adnexal masses in reproductive-aged women on the assumption that decreasing gonadotropin stimulation to a functional cyst will hasten its resolution. Either danazol (800 mg/d) or oral contraceptive pills with 50 pg estrogen are advised for any cyst suspected of being functional. Crossing the true brim of the pelvis the following important tubular structures are found. The round ligament of the uterus, the infundibulopelvic ligament, which contains the gonadal vessels and the ureter. The ovaries and fallopian tube is found between the round ligament and the infundibulopelvic ligament.
Patient Position
The patient should be in steep Trendelenburg and lithotomy position. One assistant should remain between the legs of the patient to do uterine manipulation whenever required.
Port Position
The port position should be in accordance with the baseball diamond concept. If the cyst is of the right side, one port should be in the left iliac fossa and another in the right hypochondrium.
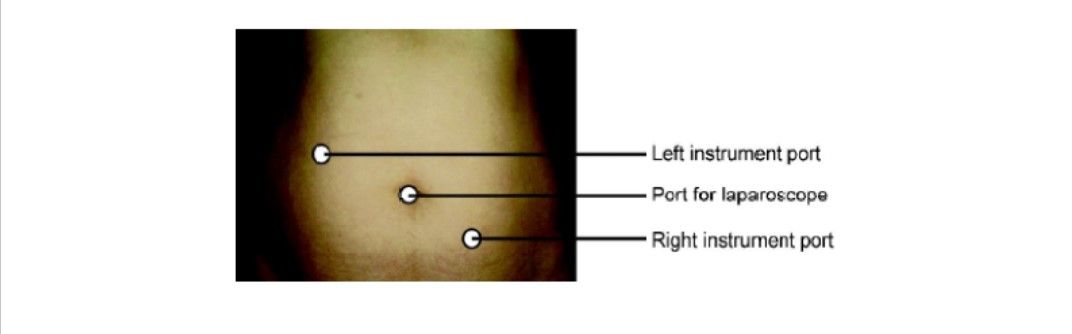
Port position for right-sided ovarian surgery
Operative Procedure
After access, the pelvis and upper abdomen have been examined, the cyst contents should be aspirated. Once the capsule is opened, the interior of the capsule is examined and suspicious areas should be sent for biopsy. The entire cyst capsule must be removed to search for an early carcinoma. Whether to perform oophorectomy or cystectomy depends on the patient’s age and characteristics of the mass.
Ovarian Cystectomy
Medical management of endometriomas has proven ineffective, either laparotomy or operative laparoscopy is necessary. Laparoscopic ovarian cystectomy removes the cyst with minimal trauma to the residual ovarian tissue. Laparotomy for ovarian cystectomy is not a good procedure because of the increased risk of ovarian adhesion formation. Three methods to manage such cysts are drainage, excision, and thermal coagulation. By excising the unruptured cyst, a histopathologic examination is more complete and the risk of recurrence is minimized, but laparoscopic removal of the intact cyst is very difficult and aspiration is recommended for functional cysts, which are diagnosed laparoscopically. Many cysts are ruptured during their manipulation despite a delicate technique.
Thermal ablation does not destroy the entire cyst wall, and the underlying ovarian cortex can be damaged by the heat. Therefore, the excision of the entire cyst wall with the help of blunt stripping and sharp dissection by scissors is recommended. The removal of a cyst 10 cm or larger is difficult laparoscopically. Aspiration before removal of large cysts is practical and can be accomplished using an 18 gauge needle passed through the separate puncture of the abdominal wall while stabilizing the cyst. The suction irrigation instrument can also be used to aspirate the content of the cyst. If gross characteristics of ovary look suspicious for malignancy. Some gynecologists recommend peritoneal washing before puncturing an ovarian cyst, because any cyst may be malignant. The peritoneal fluid or washings should be sent for cytological examination.
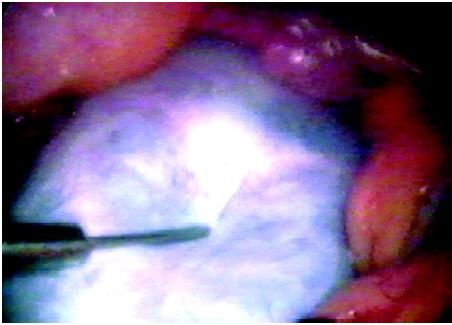
An ovarian cyst is aspirated for ovarian cystectomy
After the aspiration capsule of cyst is stripped from the ovarian stroma using two grasping forceps and the suction- irrigator probe for traction and counter traction. The electrosurgery can be used at low power to seal blood vessels at the base of the capsule and at higher powers to vaporize small remnants of a capsule. Bipolar forceps also can be used to control bleeding. The open jaw of bipolar can touch the oozing area and hemostasis can be achieved. Sometimes it is difficult to remove the capsule from the ovarian cortex so that injecting dilute vasopressin between the capsule and cortex facilitates the stripping procedure. If the cyst wall cannot be identified clearly, the edge of the ovarian incision can be “freshened” with scissors and the resulting clean edge reveals the two-layer, the outer layer will be ovarian and inner cystic. If this does not free the capsule, the base of the cyst is grasped, and traction applied to the cyst with counter traction to the ovary.
Sometimes the complete cyst or portions of the wall may be densely adherent to the ovary, requiring sharp or electrosurgical dissection to completely free the cyst wall. Generally, when the cyst capsule is removed from the ovary, the contraction of the ovarian capsule provides significant hemostasis. Bleeding can occur at the base, particularly if the cyst was close to the hilum. Under these circumstances, a needle electrode or a fine bipolar forceps can be used to minimize thermal damage. Large cysts sometimes need partial oophorectomy, to remove the distorted portion of the ovary, and the remaining cyst wall can be stripped from the ovarian stroma. Teratoma often can be excised intact but often the cyst rupture. After extraction, if the ovarian edges overlap itself, the defect is left to heal without suturing because adhesions are more likely, following the use of suture. In rare instances one or two fine, absorbable monofilament sutures may be needed to approximate the ovarian edges. The sutures are placed inside the ovary to decrease the formation of adhesions.





