A Review Article
Eleftherios Koulouteris
General Surgeon M.D, F.MAS, D.MAS
ABSTRACT
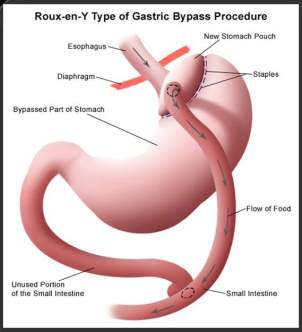
After the introduction of the laparoscopic Roux-en-Y gastric bypass (RYGB), many articles have validated that it is safe, it can be performed with out many difficulties, and is cost-effective, with decreased morbidity and similar weight loss with respect to the open technique. Advantages of laparoscopic RYGB compare to open technique include reduction of bloodloss during operation, less postoperative pain, decreased pulmonary complication rates, a shorter hospital stay, earlier return to normal activities, and a better quality of life. For these reasons, this technique is becoming popular in surgical society. There are several techniques to perform Roux-en-Y gastric bypass (RYGBP) in Laparoscopic procedures, including hand-sewn and stapled techniques. Today more and more surgeons rely on stapling devices for the gastrojejunal anastomosis (GJA). The aim of this review article is to compare end-to-end anastomosis (EEA) using circular staplers (CSA) with end-to-side anastomosis using linear staplers (LSA) at the level of gastrojejunostomy, taking in consideration all those parameters that may influence the morbidity and mortality (eg. Age, sex, BMI, co-morbitities).There are some advantages favouring one technique over the other, but in general both are feasible and easy to perform in expert hands.
KEY WARDS
Circular stapler, Linear stapler, Laparoscopy, Bariatric Surgery, Morbid Obesity, Gastrojejunostomy, Roux-en-Y Gastric Bypass
INTRODUCTION
The WHO has declared obesity as the epidemic disease of the twenty-first century. Over than 300 million people worldwide are obese [1]. After bariatric surgery there is a 29% reduction of death regarding long term risk [2]. Laparoscopic Roux-en-Y gastric bypass (RYGB) was introduced in 1994[3]. There are several advantages regarding laparoscopic RYGB vs the open technique. These include reduced lower pulmonary complication rates, shorter hospital stay, less postoperative pain, less operative blood loss, a shorter return to normal activities, and a better quality of life [4,5].However, it is technically a very demanding laparoscopic procedure. Laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most common operations for the treatment of morbid obesity. There are early complications regarding the procedure, occurring in 10–30% of patients, especially during the learning period. These are bleeding, anastomotic leak, obstruction and other intra-operative complications such as myocardial ischemia, deep vein thrombosis, pulmonary embolus, etc. Late complications include anastomotic stricture, small bowel obstruction, cholelithiasis, nutritional deficiencies, and inadequate weight loss [6-10]. Several studies suggest that the learning curve includes 100 cases for reaching morbidity rate similar to open procedures, or a significant reduction in morbidity [11-12].
One of the most challenging steps in laparoscopic bariatric surgery is to perform the gastrojejunostomy (GJ).
MATERIAL AND METHODS
There was a review of 21 articles using various search engines including Google, Pubmed, Springer link and Medline. The study was based on the institution where the study was done, the number of cases (>50 cases per article) and exclusion of articles before 2000. The patients were divided into two groups of gastrojejunal anastomotic technique, CSA or LSA, and the results were compared. Operative time, intra-operative complications, hospital stay, major and minor post-operative complications were taken in consideration.
Technique of the procedure
Patients were mechanically ventilated, using a pressure or a volume controlled setting. Standard physiologic monitoring included pulse oxymetry, electrocardiograph and non-invasive arterial blood pressure. [13,14]. The patient was placed in the supine position, the legs were split with anti- Trendelenburg position and five ports were used [15].
After placing the ports, a division of the stomach, starting 5-6 cm below the gastoesophageal junction was done with a linear stapler, thus creating a 15-30 ml proximal gastric pouch. There was a division of the small intestine 40-60 cm from the ligament of Treitz and the Roux limp was brought near the pouch for the GJA. The Y-limp was anastomosed site by site with the rest of the small intestine using a linear stapler and the enterotomy was closed in two layer hand-sewn suture. The GJA was performed using either circular (25mm) or linear (45mm) stapler [15].
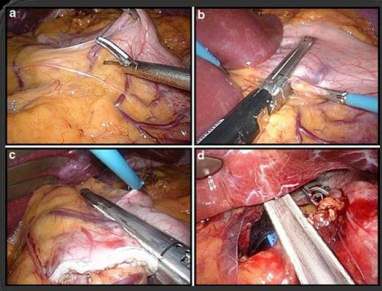
CSA technique
The CSA was performed by attaching the anvil to a guide wire or tube, and pulling the anvil of a circular stapler through the mouth and esophagus and into the gastric pouch. A gastrotomy was done and the tip of the anvil was then entered into the peritoneal cavity. The circular stapler was introduced through an extended abdominal port site, and then through an enterotomy on the afferent loop it was engaged with the anvil. The stapler was fired forming an end-to-end anastomosis and then withdrawn from the bowel and abdominal cavity. The enterotomy through which the stapler was introduced in the small intestine was then closed using a linear stapler.
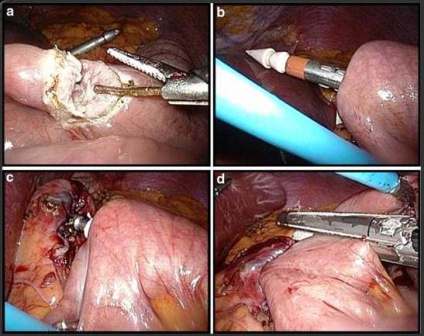
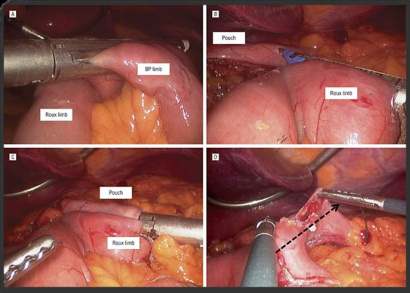
LSA technique
The LSA was performed after the creation of an enterotomy of the Roux limp and a gastrotomy of the pouch. Then the legs of the linear stapler were introduced and the stapler was fired thus creating an end-to-site anastomosis. The resultant common enterotomy was closed with a 2-layer hand-sewn suture.
After the completion of the GJA, a test was performed, using either methylene blue or air, to see the integrity of the anastomosis.
RESULTS
By reviewing the results of all articles some very interesting findings were detected. Blood loss was comparative the same between the two groups. The operative time was shorter in LSA group. The percentage of intra-operative complication was similar. The incidence of wound infection was higher in CSA group and there was a higher percentage of anastomotic strictures in the same group. Overall, there was no statistical difference regarding the post-operative complications between the two groups. There was no significant difference concerning the length of stay and the hospital costs between the two techniques. Weight loss was similar in the two groups.
DISCUSION
LRYGB is considered nowadays as the golden standard in bariatric surgery. Nevertheless, it is a challenging procedure with a significant morbidity and mortality despite the increasing surgical experience of this procedure.
Buchwald et al. in a meta-analysis has reported a mortality rate of 0.16% for LRYGB [16]. Flum et. al stated that increasing age, male sex, and non-expert surgeon are associated with a higher risk of early death after bariatric surgery [17]. The most critical post-operative complication is leak which is the most important cause of surgical related mortality resulting in peritonitis, sepsis and MOF. Male, re-do surgery, older age, a BMI >50 kg/m2 and surgeon experience are all related with poor outcome and a greater leakage rate [18 ,19]. The most frequent site for an anastomotic leak is the gastrojejunostomy[19]. There are several studies reporting an overall leakage rate ranging from 0.1% to 5.25% [19-30]. In a review of 6,135 patients in 13 selected series of laparoscopic RYGB, the mean leakage rate was 1.4% (range 0–4.3) [19]. The methylene blue test has been reported to be 100% sensitive and to have no side-effects [30]. Concerning the leakage rate, both CSA and LSA groups have similar outcome.There is no standard technique for creating the gastrojejunostomy in LRYGB. During the learning curve, the use of linear stapler may permit a lower complication rate. As a conclusion, the linear stapling technique may be faster and easier to learn. So, centres that are starting LRYG practice have to take in consideration the previous sentence. The results should be interpreted with caution because different surgeons are performing different techniques.
CONCLUSION
Both circular and linear stapled gastrogejunostomy in LRYGB is safe and easy to perform. Operative time was significantly shorter in the LSA group. Complications, length of stay, weight loss and costs were similar between the groups. CSA and LSA lead to similar early weight loss in LRYGB. In CSA group, a higher incidence of gastrojejunal strictures and wound infections were seen but there was no any statistical difference. Weight regain following LRYGBP is commonly seen in both groups. Although LSA is in favour of CSA concerning wound infection, strictures and operative time, neither linear nor circular stapled anastomosis has turned out to be superior to one another. Thus, the technique is the surgeon's choice.

REFERENCES
1. Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197–209.
2. Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N EnglJ Med. 2007;357(8):741–52.
3. Wittgrove AC, Clark GW, Tremblay LJ: Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg
4. van Gemert WG, Adang EM, Greve JW, et al. Quality of life assessment of morbidly obese patients: effect weight-reducing surgery. Am J Clin Nutr.1998;67(2):197–201.
5. Karlsson J, Sjostrom L, Sullivan M. Swedish obese subjects (SOS)–an intervention study of obesity. Two-year follow-up of health-related quality of life (HRQL) and eating behavior after gastric surgery for severe obesity. Int J Obes Relat Metab Disord. 1998;22(2):113–26.
6. Andrew CG, Hanna WH, Look D, et al: Early results after laparoscopic Roux-en-Y gastric bypass: effect of the learning curve. Can J Surg 2006;49:417–421
7. Schaeffer DF, Rusnak CH, AmsonBJ: Laparoscopic Roux-en-Y gastric bypass surgery: initial results of 120 consecutive patients at a single British Columbia surgical center. Am J Surg 2008;195:565–569
8. Huang CK, Lee YC, Hung CM et al: Laparoscopic Roux-en-Y gastric bypass for morbidity obese Chinese patients: learning curve, advocacy and complications. Obes Surg2008;18:776–781
9. Søvik TT, Aasheim ET, Kristinsson J et al: Establishing laparoscopic Roux-en-Y gastric bypass: perioperative outcome and characteristics of the learning curve. Obes Surg 2009;19(2): 158–165
10. Pournaras DJ, Jafferbhoy S, Titcomb DR et al: Three hundred Laparoscopic Roux-en-Y gastric bypasses: managing the learning curve in higher risk patients. Obes Surg 2009 Jul 23. Epub PMID: 19629602
11. Schauer P, Ikramuddin S, Hamad G, et al: The learning curve for laparoscopic Roux-en-Y gastric bypass in 100 cases. Surg Endosc2003;17:212–215
12. Shikora SA, Kim JJ, Tarnoff ME, et al: Laparoscopic Roux-en-Y gastric bypass: results and learning curve of a high-volume academic program. Arch Surg 2005;140:362–367
13. Mulier JP, Sels A, Dillemans B. Use of pressure support ventilation during laparoscopic bariatric surgery. Eur J Anesthesiology. 2008;25(S44):78.
14. Mulier JP, Dillemans B, Feryn T, et al. Adominal physiology and its impact on laparoscopic bariatric surgery. Obes Surg. 2008; 18:443.
15. Madan AK, Harper JL, Tichansky DS: Techniques of laparoscopic gastric bypass: on-line survey of American Society for Bariatric Surgery practicing surgeons. Surg Obes Rel Dis 2008; 4:166–173
16. Buchwald H, Estok R, Fahrbach K, et al. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142(4):621–32.
17. Flum DR, Salem L, Elrod JA, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294(15):1903–8.
18. Nguyen NT, Rivers R, Wolfe BM. Factors associated with operative outcomes in laparoscopic gastric bypass. J Am Coll Surg. 2003;197(4):548–55. discussion555-7.
19. Gonzalez R, Nelson LG, Gallagher SF, et al. Anastomotic leaks after laparoscopic gastric bypass. Obes Surg. 2004;14(10):1299–307.
20. Marshall JS, Srivastava A, Gupta SK, et al. Roux-en-Y gastric bypass leak complications. Arch Surg. 2003;138(5):520–3. Discussion 523-4.
21. Carrasquilla C, English WJ, Esposito P, et al. Total stapled, total intra-abdominal (TSTI) laparoscopic Roux-en-Y gastric bypass: one leak in 1000 cases. Obes Surg. 2004;14(5):613–7.
22. Madan AK, Lanier B, Tichansky DS. Laparoscopic repair of gastrointestinal leaks after laparoscopic gastric bypass. Am Surg. 2006;72(7):586–90. discussion 590-1.
23. Lee S, Carmody B, Wolfe L, et al. Effect of location and speed of diagnosis on anastomotic leak outcomes in 3828 gastric bypass cases. J Gastrointest Surg. 2007;11(6):708–13.
24. Hamilton EC, Sims TL, Hamilton TT, et al. Clinical predictors of leak after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2003;17(5):679–84.
25. Gonzalez R, Sarr MG, Smith CD, et al. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg. 2007;204(1):47–55.
26. Durak E, Inabnet WB, Schrope B, et al. Incidence and management of enteric leaks after gastric bypass for morbid obesity during a 10- year period. Surg Obes Relat Dis. 2008;4(3):389–93.
27. DeMaria EJ, Sugerman HJ, Kellum JM, et al. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg. 2002;235(5):640–5. discussion 645-7. OBES SURG
28. Carucci LR, Turner MA, Conklin RC, et al. Roux-en-Y gastric bypass surgery for morbid obesity: evaluation of postoperative extraluminal leaks with upper gastrointestinal series. Radiology. 2006;238(1):119-27.
29. Ballesta C, Berindoague R, Cabrera M, et al. Management of anastomotic leaks after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18(6):623–30.
30. Christian DJ, Barba C, Burke-Martindale C, et al. A simple bedside evaluation to detect gastroesophageal leaks after gastric bypass. Surg Endosc. 2004;18:S193. (abst).





