
LAPAROSCOPIC MANAGEMENT OF VAULT PROLAPSE
Member of world association of laparoscopic surgeons
Project submitted toward completion of diploma in minimal access surgery ,World Laparoscopy Hospital, Gurugram, NCR Delhi .India ,august2007
DR NAHED AL TABAS, MRCOG, D.MAS Gynacologisst and obstatrion
MEMBER WORLD ASSOCIATION OF LAPAROSCOPIC SURGEON
Project Submitted Towards Completion Of Diploma In Minimal Access Surgery, World Laparoscopy Hospital, Gurugram, NCR Delhi, India. AUGUST 2007.
Abstract :
Repair of vaginal vault prolapse remains a surgical challenge. Abdominal, vaginal, and combined procedures have been described. The ideal operation remains elusive with regard to outcomes, morbidity, and economics. As an extension of the abdominal approach, laparoscopy continues to gain favor as an access method and as a surgical advancement. Recent studies highlight a number of laparoscopic techniques for restoration of apical support that demonstrate feasibility and encouraging results. Further study is necessary to determine if the minimally invasive nature of laparoscopy can duplicate or surpass standard abdominal and vaginal approaches to the repair of pelvic organ prolapse.
Aim :
The prevalence of pelvic prolapse should continue to increase as our population ages. With the increased prevalence will come a greater need to evaluate and treat women with symptomatic vault prolapse. This review focuses on prolapse of the vaginal vault and discusses the evaluation and surgical therapies including vaginal, abdominal, and laparoscopic approaches
Keywords :
vaginal vault prolapse, cystocele rectocele, enterocele, cystourethrocele, anatomy pathology, management of vaginal vault prolapse, laparoscopic role in the management of vaginal vault prolapse
Definition and classification :
Vaginal vault prolapse refers to a herniated of vaginal vault apex or when the upper portion of the vagina loses its normal shape and sags or drops down into the vaginal canal or outside of the vagina. It may occur alone or along with prolapse of the bladder or uretha, small intestine or rectum. These displacements are typically graded on a scale of 0 to 4, with 0 referring to no prolapse, 1 halfway to the hymen, 2 at the hymen, 3 halfway out of the hymen reducable and 4 referring to total prolapse irreducible (ie, procidentia)
Other classification mild, moderate and sever
Terms used to describe specific types of female genital prolapse include:
- Cystocele: hernia of the bladder with associated descent of the anterior vaginal segment.
- Cystourethrocele: a cystocele combined with distal prolapse of the urethra (bladder neck) with or without associated urethral hypermobility..
- Vaginal vault prolapse: descent of the vaginal apex (following hysterectomy) into the lower vagina, to the hymenal ring, or through the vaginal introitus.
- Rectocele: hernia of the rectum with associated descent of the posterior vaginal segment.
- Enterocele: herniation of the small bowel/peritoneum into the vaginal lumen, most commonly presenting following hysterectomy in conjunction with vaginal vault prolapse
Incidence :
The rate of vaginal vault prolapse after hysterectomy which was done due to other than uterine prolapse is only 1.8%, while the incidence after hysterectomy due to uterine prolapse is reported to be 11.6%, but aging of the population will further increase the number of women affected. This significant difference clearly indicates that if the ligaments were too weak to support the uterus, they are often also too weak to support the vaginal vault.
Anatomy : (10-11)
Under standing of anatomy of pelvic supports help in diagnosis and anatomical restoration and surgical correction. The vagina is flattened fibromuscular tube lined by vaginal epithelium and enveloped by endopelvic fascia. This vaginal fascial sheath is attached to deeper superior and posterior sheath supports. De Lencey described three levels of vaginal supports.
1-The upper quarter level (1) is suspended by the cardinal/uterosacral ligament
2-The middle two quarter level2 is maintained by lateral attachment anteriorly to the arcus tendinous fascia pelvis and posterior to pubococcygeus and iliococcygeus fascia
3-The lower quarter of the vagina (level3) is maintained by fusion of the lower vagina to the urogenital diaphragm anteriorly and perineal body posteriorly.
In addition the vagina has structural integrity provided by the pubocervical fascia anteriorly and rectovaginal fascia posteriorly . The pubocervical fascia is attached superiorly to the pericervical ring at the level of external cervical os caudally to the urogenital diaphragm and laterally to the arcus tendinous and fascia pelvis posteriorly . The rectovaginal fascia is attached caudally to the perineal body superiorly it merges into cardinal \ uterosacral ligament and laterally it merges with parietal fascia covering the iliococcygeus and pubococcygeus muscle. These three types of support suspension attachment and fusion are continuous with one another and interdependent. They maintain adequate vaginal length, centrally poisoned in the pelvis and horizontally oriented above the pelvic floor muscle so that at times of increase intra abdominal pressure the perpendicularly pushing down force applied to the vagina is counteracted by pressure from the pelvic diaphragm, the vagina is compressed by these two opposing forces and remain in place.
Pathology : (6)
Vaginal vault prolapsed is caused by:
1-attenuation of cardinal\ uterosacral ligament complex when they are excised during hysterectomy
2-separation of pubocervical fascia from rectovaginal fascia
3-separation of pubocervical fascia rectovaginal fascia from the cardinal\ uterosacral ligament complex.
These cause loss of suspension of level 1.The type of posthysterectomy prolapse that will occur depend on which level of support has failed. Defective suspension of the vaginal apex level1 with preservation of mid vaginal support level2 presents as simple eversion of upper vagina which always associated with cyctocele and\or rectocele and this called complex vaginal eversion.
Vaginal vault prolapse is often complex
Symptoms : (12)
1-A feeling of pelvic fullness or pressure or heaveness.
2-A feeling as if something (mass) protruding out of the vagina.
3-A pulling or stretching in the groin area or a low backache.
4-Painful intercourse (dyspareunia).
5-Spotting or bleeding from the vagina due to vaginal erosion or Bleeding from mucosal ulcerations or from the cervical .
6-Urinary problems, such as involuntary release of urine (stress incontinence )or a frequent or urgent need to urinate, , recurrent urinary infections, inability to empty the bladder, difficulty in micturate,. or the need to digitally reduce (splint) the prolapse in order to urinate .
7-Difficulty with bowel movements, such as constipation or needing to support the back of the vagina to have a bowel movement.
8- The symptoms usually worsen with exertion and ease with bed rest.
Risk Factors : (3)
The majority of patients with clinically significant prolapse will have at least two or more risk factors for the disorder, which cumulatively over time, contribute to worsening prolapse as a women ages. Purported risk factors for pelvic organ prolapse include
1- Multiparty
2-Operative vaginal delivery
3- Obesity
4- Advanced age (old age)
5- Estrogen deficiency
6- Neurogenic dysfunction of the pelvic floor, or prior pelvic surgery with disruption of natural support or Conditions affecting the spinal cord, and spinal cord injury, that cause paralyses of the muscles of the pelvic floor
7-Connective tissue disorders
8- Chronically increased intra-abdominal pressure (eg, from strenuous physical activity or coughing).7@
Prevention :
1-Maintain a healthy body weight.
2-Exercise regularly (for 20 to 30 minutes, three to five times per week), including Kegel exercises (up to four times a day).
3-Eat a healthy diet balanced in protein, fat and carbohydrates and high in dietary fiber .
4- Smoking cessation reduces the risk of developing a chronic cough, which can put extra strain on the pelvic muscles.
5-Consider estrogen replacement therapy after menopause.
6-Use correct lifting techniques
7-During hysterectomy the uterosacral and cardinal ligaments must be carefully ligated and tied together and the cul-de-sac must be obliterated to reduce the risk of subsequent enterocele and to suspend the vaginal vault properly.
Diagnosis :
It's very common to have more than one type of prolapse at the same time and each one should be taken into consideration when planning treatment. Diagnosis is generally straight forward, taking the history from the patient with a pelvic examination demonstrating prolapse of the vaginal apex (Fig. 1). It is important to demonstrate any associated conditions such as cystocele (central and lateral defects), enterocele, or rectocele because they will need to be repaired at the time of surgery. Ultrasound to the pelvis and MRI (magnetic resonance imaging) can help in the diagnoses. Additionally, in severe cases, an IVP (intra venous pyelogram) or renal ultrasound or Cystourethroscopy, or cystoscopy should be performed to demonstrate possible ureteral obstruction from the severe ureteral angulation's that can occur. In rare cases, a ureteral stent must be in place until the time of operation
Treatment :
Treatment devided into non surgical and surgical
Important considerations for non-surgical or surgical decision making (16)
- Medical condition and age of the patient
- Severity of symptoms
- Patient's choice (ie, surgery or no surgery)
- Patient's suitability for surgery
- Presence of other pelvic conditions requiring simultaneous treatment, including urinary or fecal incontinence
- Presence or absence of urethral hypermobility
- Presence or absence of pelvic floor neuropathy
- History of previous pelvic surgery
Non surgical (conservative) :
Physiotherapy :
If the prolapse is mild or moderate pelvic floor exercises (kegel exercise) can be benefit. It may take a few months before notice any improvement
Estrogen replacement therapy (ERT) :
Oestrogen cream can be used temporarily for a month or two before and after operation or in patient unfit for operation can be also used with the pessary. This helps to strength vaginal and pelvic tissues and may improve the outcome of surgery .
Vaginal pessaries :
A vaginal pessary is a small device, similar to a diaphragm or cervical cap, which is inserted into the vagina to hold the prolapsed organ(s) in place. Pessaries are made of latex or silicone and come in many different shapes and sizes. Pessaries are generally recommended as treatment for women who are waiting for surgery, and women who are unable or choose not to have surgery9@
Surgery : (10)
The aims of surgery for vaginal vault prolepses are
to correct the anatomical defects, preserve vaginal function and
Improve symptoms with as low a risk of recurrence as possible. Any treatment achieves a result where 80% of women are still symptom-free after five years would be considered a good result.
There are five surgical approaches: (13)
1-Vaginal Approach: This is the traditional first-line approach for prolapse and may still be the preferred route for elderly and debilitated women. It is difficult to suspend the vagina to a higher level with maintenance of vaginal length by this approach and the recurrence of vault prolapse in the literature is between thirty to fifty percent in five years.
2-Abdominal Approach by Incision (laparotomy): This approach is often used after repeated failures of vaginal surgery for vault prolapse and a synthetic mesh is usually used to attach the vagina to the front of the sacral bone (sacrocolpopexy). This approach is also used primarily for cystocele cause by lateral defects and the operation is called a paravaginal repair. These techniques tend to lengthen and support the vagina in a more anatomical position and in the literature have higher success rates at five years than the vaginal approach.
3-The Laparoscopic Approach: This approach reproduces the same surgery as by laparotomy but through tiny incisions with resultant less pain, morbidity, and hospital stay.
4-Robotic Surgery:Robot-assisted laparoscopic surgery is an effective alternative to traditional surgery for treatment of vaginal vault prolapse, U.S. researcher report.
Robotic surgery involves the use of a device that helps speed up the repair and simplifies technically difficult aspects of vaginal vault prolapse surgery. 2@ In the new robotic approach, the surgeon operates remotely from a computer terminal, guiding the robotic hand that performs the surgery, rather than standing over the patient This technique also offers 3-D vision, better ability to maneuver and reduction of any tremor that might be present in the human hand.
5. A combined vaginal/laparoscopic approach to sacrocolpopexy appears to be effective and associated with a low risk of intraoperative and postoperative morbidity . Its principal advantage over a completely laparoscopic approach is in removing the technical demands of laparoscopic suturing1
Vaginal operation : (11_12)
Vaginal approach started first to avoid the need for laparotomy, it has fewer complications, less blood loss and postoperative discomfort, a shorter hospital stay, and less expense.
1-Sacrospinous ligament fixation :
Technique :
Nichols described the need to penetrate the right rectal pillar into the pararectal space near the ischial spine. The next step is grasping the ligament and muscle with a long Babcock clamp. Place two #2 polyglycolic sutures through the sacrospinous ligament, 1.5 to 2 fingerbreadths medial to the ischial spine. Attach 1 end of the suture to the undersurface of the posterior vaginal wall at the apical area. When the posterior colporrhaphy reaches the midportion of the vagina, tie the sacrospinous suspension sutures, firmly attaching the vaginal apex to the surface of the coccygeal-sacrospinous ligament complex with no intervening suture bridge (FIGURE 1 ).
Modifications :
The most notable modification is the Miyazaki technique, which substitutes the Miya hook for the DesChamps ligature carrier. The Miya hook is reportedly safer for the pudendal complex, which may lie up to 5.5 cm medial to the ischial spine. 7 The path of the Miya hook avoids Alcock's canal and its neurovascular pudendal bundle.
The Caprio ligature carrier (Boston Scientific, Boston , Mass ) is also useful for the placement of sacrospinous sutures; unlike the Miya hook, however, the Caprio ligature carrier is a disposable instrument and thus is not reusable.
Complications : hemorrhage, pudendal nerve injury, rectal or bladder injury, and recurrent anterior vaginal wall prolapse.
FIGURE 1 2 "pulley stitches" secure the apex
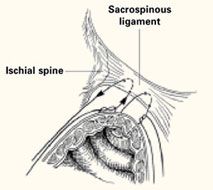
Place 2 nonabsorbable monofilament "pulley stitches" to secure the vaginal apex to the ligament.
2-Iliococcygeal fixation
Technique :
Open the posterior vaginal wall in the midline, as if preparing to perform a posterior colporrhaphy. Develop the rectovaginal spaces bluntly and bilaterally-laterally toward the levator muscles and posteriorally toward the ischial spines. Use the nondominant hand to depress the rectum downward and medially, and place a single #0 polyglycolic suture deep into the iliococcygeus muscle and fascia at a point 1 to 2 cm caudad and posterior to the ischial spine. Then pass both ends of the suture through the ipsilateral posterior vaginal apex and hold them with a hemostat. Repeat the procedure contralaterally.
Usually no vaginal epithelium needs excision because the upper vagina is attached bilaterally, resulting in good vaginal length and circumference. When posterior colporrhaphy is completed and the posterior vaginal wall is closed, tie both iliococcygeal-fixation sutures in place.
Complications emorrhage , bladder/rectal perforation , and recurrent vault prolapse .
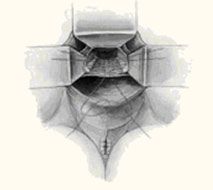
3-Modified McCall culdoplasty :
Technique :
Excise an elliptical wedge of mucosa from the anterior and posterior walls of the prolapsed vagina to narrow the vault and allow access to the lateral fascial supports of the vagina and rectum. The width and length of the excised wedges are determined by the desired dimensions of the reconstructed vagina.
After isolating and excising the enterocele sac, place up to 3 modified McCall stitches, each one slightly higher than its predecessor. Each suture should incorporate the full thickness of the posterior vaginal wall, the cul-de-sac peritoneum, the remains of the uterosacral-cardinal complex bilaterally, and the fascial tissue lateral and posterior to the upper vagina and rectum (FIGURE 2 ).
Once they are in place, tie the sutures in the opposite order in which they were placed. These stitches fix the prolapsed vaginal vault to the uppermost portion of the endopelvic fascia at the same time as they accomplish a high closure of the culdesac peritoneum.
In the classic McCall culdoplasty shown here, only the distal-most suture incorporates the posterior vaginal wall. With the "modified" technique, however, all sutures incorporate the full thickness of the posterior vaginal wall, as well as the cul-de-sac peritoneum, the remnants of the uterosacral-cardinal complex bilaterally, and the fascial tissue lateral and posterior to the upper vagina and rectum .
Complication: recurrent vault prolapse and new-onset dyspareunia.
FIGURE 2
Classic vs modified McCall culdoplasty
3-High uterosacral ligament suspension with fascial reconstruction
Technique :
Grasp the vaginal apex with 2 Allis clamps and incise it with a scalpel. If an enterocele sac is present, dissect it off the vaginal epithelium to the neck of the hernia, open it, and then excise it. Place a delayed absorbable or permanent pursestring suture about the neck of the hernia to close the peritoneal defect. If an anterior colporrhaphy or sling is required, perform them at this time.
Place a moist laparotomy pad in the cul-de-sac, and insert and elevate a Deaver retractor to remove the intestines from the cul-de-sac and improve exposure. Next, palpate the ischial spines transperitoneally.
Once the spines are identified, the remnants of the uterosacral ligaments can be identified posterior and medial to the spines and can be palpated transperitoneally or transrectally. Remember that the ureters are also quite close to the ischial spines at this location, running along the lateral pelvic sidewall 2 to 5 cm ventral and lateral to the ischial spines.
After identifying the uterosacral ligaments, grasp their remnants with Allis clamps and place 2 to 3 delayed absorbable or permanent sutures through the rectovaginal fascia of the inner posterior vaginal wall epithelium at one lateral vaginal apex, through the ipsilateral plicated uterosacral ligament complex, and then through the pubocervical fascia of the anterior vaginal wall of the ipsilateral vaginal apex. Hold these sutures while performing the same procedure contra laterally ( FIGURE 3 ). Close the apex and tie these sutures in place, suspending the corners of the vaginal apex from the uterosacral complex bilaterally, and restoring the continuity of the paracervical ring (FIGURES 4 , 5 ).
Benefits of this technique include:
- Preservation of adequate vaginal length,
- Reduced risk of nerve injury, and
- Restored continuity of the paracervical ring when the pelvic pararectal, uterosacral, and pubocervical fascia are reapproximated circumferentially.
Complication : potential for ureteral kinking or obstruction. Thus, it is prudent to perform cystoscopy after this procedure to rule out occult injury.
FIGURE 3 Suspend apical corners bilaterally
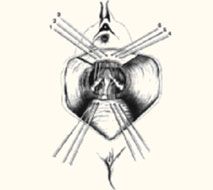
The corners of the vaginal apex are suspended from the cardinal-uterosacral complex bilaterally, with all sutures placed posterior and medial to the ischial spines. Copyright 1998 by C.G. Bachofen.
FIGURE 4
Suture placement penetrates multiple layers
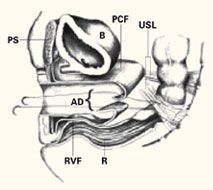
Sagittal view of correct suture placement. PS=pubic symphysis, B=bladder, PCF=pubocervical fascia, USL=uterosacral ligaments, AD=apical defect, RVF=rectovaginal fascia, R=rectum. Copyright 1998 by C.G. Bachofen.
FIGURE 5
Suspend the fascia from uterosacral ligaments
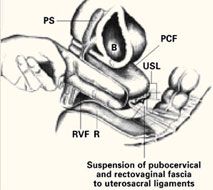
Sagittal view after tying of sutures. Note restoration of the normal anatomic axis. PS=pubic symphysis, B=bladder, PCF=pubocervical fascia, USL=uterosacral ligaments, RVF=rectovaginal fascia, R=rectum. Copyright 1998 by C.G. Bachofen.
5-Posterior intravaginal slingplasty (IVS) (17)
Technique :
Introduced as the infracoccygeal sacropexy, the posterior intravaginal slingplasty (Posterior IVS, Tyco/U.S. Surgical, Norwalk , CT ) is a novel minimally invasive technique using a polypropylene tape for treating vaginal vault prolapse in a fashion analogous to the anti incontinence tension-free vaginal tape procedure. This procedure recreates a central suspensory ligament at the level of the ischial spines, analogous to the cardinal ligaments, with a synthetic tape to restore vault support. For the posterior intravaginal slingplasty, a posterior vaginal dissection is performed to the level of the vaginal apex. The tape is placed through bilateral pararectal incisions about 3 cm lateral and posterior to the anus. A metal tunneller is guided through the levator muscles and into the endopelvic fascia over the iliococcygeus muscle or immediately anterior to the ischial spine and sacrospinous ligament. The tape is secured to the vaginal apex and adjusted to provide vault support.
Complication :
rectal perforation and rectal tape erosion were noted.
6-Tight (anterior and posterior) repair
This procedure is rarely done. It involves removing a large amount of the vaginal tissue in order to tighten and support the vagina. The main complication of this operation is severe pain.
7-Colpocleisis (colpectomy or Le Forts procedure)
Colpocleisis - vaginal closure - is procedure that is rarely done. It closes off the vagina by stitching the front and back walls together, leaving two pencil-width channels on either side. The operation is performed vaginally and can be done using a local anesthetic or epidural.
It is only offered as a treatment option for women who have severe prolapse, are too frail to undergo any other surgical treatment and are absolutely certain they don't ever want to have sexual intercourse again, in recurrent cases, and in very old women
Benefit : (10b) No recurrent, less complication and fast operation can be done under local anesthesia
Risk : no intercourse
Abdominal operation
Abdominal operation devided into laparotomy and laparoscopy both same operations except in laparotomy abdominal incision is 8-10 cm while laparoscopy is only 3 punctures each 0.5-1 cm
1-High uterosacral ligament suspension :
Technique :
Identify and tag the remnants of the uterosacral ligaments at the level of the ischial spines. Once the ureters are identified and isolated, address the enterocele by obliterating the cul-de-sac via Halban's culdoplasty or abdominal McCall's culdoplasty. Open the peritoneum over the vaginal apex and trim it back to the level of the endopelvic fascia of the vaginal wall. After excising the redundant peritoneum of the vaginal apex, identify and reapproximate the pubocervical fascia of the anterior vaginal wall and the rectovaginal fascia of the posterior vaginal wall using interrupted or running nonabsorbable suture.
Then use nonabsorbable sutures to suspend each corner of the prolapsed vagina from its respective ipsilateral uterosacral ligament.
Complication: less chance of ureter kinking or injury
2-Abdominal sacral colpopexy
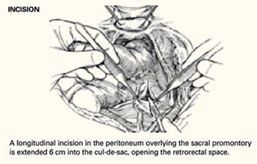
Technique Reflect the sigmoid colon as far as possible into the left lateral pelvis to expose the sacral promontory. If it has not already been done, free all adhesions between the colon and pelvic peritoneum to fully mobilize the colon and permit its maximal retraction out of the pelvic field prior to making the peritoneal incision.
Also make it a point to identify all structures at risk during this portion of the procedure-namely, the common iliac vessels, ureters, and middle sacral artery and vein. The left common iliac vein is medial to the left common iliac artery and is particularly susceptible to injury during this phase of the procedure.
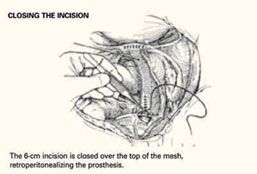
Make a longitudinal incision in the peritoneum overlying the sacral promontory and extend it approximately 6 cm from the promontory dorsally into the cul-de-sac, opening the retrorectal space ( FIGURE 1 ). Using a fine tonsil forceps and cautery, very gently dissect the retroareolar filmy tissue overlying the anterior longitudinal ligament away from S1 in thin layers until the white periosteum of the anterior longitudinal ligament overlying S1 is clearly exposed. It now becomes very easy to visualize the course of the middle sacral artery and vein. With these vessels under direct visualization, place 2 permanent #0 sutures through the periosteum of S1.
Insert a probe such as an end-to-end anastomotic sizer or handheld Harrington retractor into the vagina and extend it, elongating and elevating the vaginal cylinder. It now becomes much easier to identify the interface between the bladder and vagina prior to making the peritoneal incision.
If the interface remains indistinct, instill 150 cc of saline into the bladder to delineate its boundaries. Then elevate and incise the vesicouterine peritoneum overlying the junction between the bladder and vaginal apex; this provides access to the vesicocervical space. Dissect the bladder off the anterior vaginal wall in a caudal direction until the pubocervical fascia can be identified. Do not dissect away the peritoneum over the posterior vaginal wall, but leave it intact .
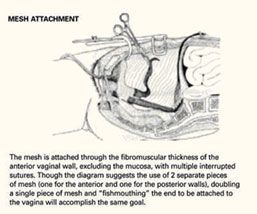
Reconstructive materials :
Fold a piece of 5-inch mesh over into itself and suture the layers together to create a double-thickness configuration. Then "fishmouth" the caudal end of this mesh prosthesis, producing both an anterior and posterior leaf. With the obturator still within the vaginal cylinder stretching the vaginal apex, secure the posterior leaf of the mesh to the posterior vaginal wall with 3 to 5 nonabsorbable #0 sutures.
Boul adhesion, rectocele , dyschasia, and prolapse other site of operation, mesh erosion, bleeding from the sacral promontory and
postoperative ileus. The risk of bleeding can be minimized by the use of bone anchors on the sacral promontory .(19)
3-Paravaginal defect repair
Technique :
Enter and gently develop the retropubic space of Retzius, taking care not to disrupt the myriad venous anastomotic networks of the plexus of Santorini, located on and around the bladder. Bluntly mobilize the bladder bilaterally, exposing the lateral retropubic spaces, the pubococcygeus and obturator internus muscles, and the obturator neurovascular bundles. Within each retropubic space, palpate the ischial spine. Then visualize the arcus, seen as a white ligamentous band, as it courses from the ischial spine caudally toward the ipsilateral posterior pubic symphysis. A lateral paravaginal defect representing avulsion of the vagina off the arcus tendineus fascia pelvis, or of the arcus tendineus fascia pelvis off the obturator internus muscle, can now be visualized.
While gently reflecting the bladder medially with a wide ribbon, insert a few fingers of the nondominant hand into the vagina and elevate the ipsilateral anterolateral vaginal sulcus. Then place a suture through the fibromuscular thickness of the lateral vaginal apex, just above the uplifting fingers in the vagina, and then slightly cephalad into the arcus tendineus fascia pelvis or obturator internus fascia on the pelvic sidewall, at a point 1 to 2 cm distal to the ischial spine. Place 3 to 5 additional sutures in a similar fashion at 1-cm intervals. The most distal suture should be placed as close as possible to the pubic ramus into the pubourethral ligament. If necessary, repeat the procedure on the contralateral side. Then tie all sutures into place, thereby completing the repair.
Complication : injury to the bladder
Materials and Methods :
A literature search was performed using Medline and search engine Google to find related articles. The following search words were used: vaginal vault, vaginal vault prolapse, management of vaginal vault prolapse, laparoscopic role in the management of vaginal vault prolapse.
Vaginal vs abdominal route :
1- Benson et al did study (Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. .Eighty women ( vaginal 42, abdominal 38) found that, after 5 years of follow-up, women managed vaginally had a 6-fold increased incidence of recurrent vault prolapse, a 3-fold increased incidence of recurrent cystocele, and twice the reoperation rate, compared with women whose initial repair was abdominal.In the study, 48 women with total vault prolapse underwent vaginal bilateral sacrospinous fixation and paravaginal defect repair, and 40 underwent abdominal sacral colpopexy and paravaginal defect repair. Although the vaginal approach was associated with a shorter operative time and decreased hospital stay in the short term, it necessitated longer postoperative catheter use and was associated with more urinary tract infections and postoperative incontinence and a higher overall failure rate . (9)
2- Sze and colleagues 24 addressed a similar question in retrospective fashion, reviewing the medical records of 117 women surgically treated for total vault prolapse. Sixty-one women underwent vaginal sacrospinous ligament fixation and Raz urethropexy, while 56 underwent abdominal sacral colpopexy and Burch urethropexy. After a mean follow-up of 24 months, 33% of the women managed vaginally developed recurrent pelvic organ prolapse, compared with only 19% of the women managed abdominally. In addition, 26% of the women managed vaginally had recurrent urinary incontinence, compared with only 13% of the women managed abdominally.
3-A separate randomized, prospective study by Maher et al 22 compared abdominal sacral colpopexy (n=47) and vaginal sacrospinous ligament fixation (n=48) for stage II to IV vault prolapse. After a mean follow-up of 2 years, subjective and objective success rates did not differ significantly between the 2 routes.
4-Beer M, Kuhn A, searched MEDLINE for articles indexed between 1972 and 2002 and dealing on operative techniques for vault prolapse. They found 149 articles describing, variously, abdominal sacrocolpopexy with mesh (2008 patients), other transabdominal methods (387 patients), sacrospinous ligament fixation (2390 patients), other transvaginal repairs (1556 patients), laparoscopic procedures (128 patients), intravaginal sling (168 patients) and vaginal obliteration techniques (157 patients). Two procedures are more frequently used than the others: abdominal sacrocolpopexy and transvaginal sacrospinous ligament fixation. They were unable to detect any differences in the complication and/or cure rates, but did find a slightly better long-term anatomical outcome after the abdominal technique. Since no standardized outcome measure is available it is difficult to compare the functional results. Only in more recent studies have subjective cure rates (patient satisfaction with the outcome) also been evaluated as well as the objective cure rates determined by the investigators, and the objective and subjective rates are not necessarily the same. The subjective cure rate is probably more strongly influenced by the functional outcome in terms of micturition, defaecation and sexual activity than by the anatomical result .(15)
5-Shull and colleagues 20 studied 42 women who underwent suspension of the vaginal cuff to iliococcygeus fascia and repair of coexisting pelvic support defects. Of these women, 2 (5%) had recurrence of their cuff prolapse during follow-up, one of whom required further surgery (she also had recurrence of an inguinal hernia that had been repaired at the original surgery). The other patient, who had undergone 5 previous pelvic procedures, developed asymptomatic prolapse of the cuff halfway to the hymen. Six additional patients had loss of support at other sites in the follow-up period, one of whom required repeat surgery. Ninety-five percent of women experienced no persistence or recurrence of cuff prolapse 6 weeks to 5 years after the procedure.
6-Meeks and colleagues 21 also applied the Inmon technique in 110 women with posthysterectomy vault prolapse or total uterine procidentia. In both studies, the most commonly reported complications. Included hemorrhage (1.2%), bladder/rectal perforation (1.2%), and recurrent vault prolapse (8%).
7-Sze and Karram 13 found in Modified McCall culdoplastyan 11.5% incidence of recurrent vault prolapse and an associated 22% incidence of new-onset dyspareunia. infracoccygeal sacropexy, is a minimally invasive, transperineal approach to vaginal vault prolapse. The anatomic and physiologic concepts are similar to those of the tension-free vaginal tape (Gynecare, Somerville , NJ ) in the treatment of stress incontinence. However, because it is a new procedure, further evaluation is needed before it can be adopted into clinical practice.
8- Farnsworth did study in posterior intravaginal slingplasty (IVS) as an outpatient surgery. In the initial case series of 93 patients collected, 1 rectal perforation and 1 rectal tape erosion were noted as a complication .(23)
9- Dr. Jim W. RossA did prospective study of 37 women with post hysterectomy vault prolapse had sacrocolpopexy utilizing Prolene mesh he found all 37 patients (mean age 66 and parity 3) had an intact apical vault at 3 months. Four patients had detrusor instability. One partial small bowel obstruction developed at two weeks, secondary to bowel adhering to the mesh. Twenty-nine patients were seen at 5-years. Twenty-seven had intact apical vaginal vaults (93%). Twenty-three (79%) were continent. Four (14%) of the six patients with genuine stress incontinence had detrusor instability. Grade I, II, and III anterior wall prolapse occurred in 3 (10%), 4 (14%), and 1 (3%) patients, respectively. Grade I, II, and III rectoceles were present in seven (24%), 3 (10%), and 2 (7%) patients. Both Grade III and two Grade II patients with rectoceles were symptomatic, three with rectal splinting and one with dyschezia. Five patients (17%) complained of obstructive defecation. Nine of the patients with anterior or posterior wall prolapse did not have an apical vault repair . (18)
Discussion :
The abdominal procedure is better than vaginal operation because
1-The traditional surgical procedure for vaginal management of total vault prolapse-sacrospinous ligament fixation-distorts the axis of the vagina.
2-Native tissues are not as strong as synthetic materials. In postmenopausal women, a repair in which the thin, atrophic vaginal apex is secured to the sacrospinous ligament will not have the same durability as a repair involving mesh.
3-In vaginal paravaginal repair, the extensive periurethral dissection required can damage fine branches of the pudendal nerve that innervate and control the urethral sphincter. Such extensive dissection is not required for paravaginal repair from the abdominal approach.
4- In the vaginal approach, it can be difficult to gain adequate exposure high in the retroperitoneum to reattach the endopelvic fascia of the vaginal apex to the arcus at its origin just distal to the ischial spine.
5-Vaginal sacrospinous ligament fixation report a roughly 20% incidence of recurrent or persistent anterior vaginal wall relaxation, or symptomatic cystocele, within 1 year after the surgery. Alteration of the vaginal axis in an exaggerated posterolateral direction after this procedure is thought to place undue tension on the anterior segment of the vaginal wall and predispose women to prolapse at a site opposite the repair. iliococcygeus fixation is technically easier and places less tension on the anterior vaginal wall.
6-Abdominal operation(laparoscopy and laparotomy ) has less complication and recurrent rate, because they gives better vision and clearer definition of fascial defects thus allowing rational repair. The principle of treatment is the same for both.
7-Laparoscopy has more benefit than laparotomy in
Factor
Laparatomy
Laparoscopic
Hospital Stay
1-2 weeks
1-2 days
Pain during recovery
Moderate
Minimal
Return to work timeframe
4 weeks
1-2 weeks
Cosmetic results
4-5" scar
3 tiny incisions
Summary :
There are three primary routes of access in reconstructive pelvic surgery (abdominal, vaginal and laparoscopic) for the repair of anterior, superior and posterior defects; the choice often depends on the surgeon's experience. Of the abdominal repairs, abdominal sacrocolpopexy with mesh remains the 'gold standard'; the retropubic paravaginal repair and laparoscopic techniques have not gained widespread acceptance. The laparoscopic approach appears to be the least utilized, because of the great degree of technical difficulty associated with laparoscopic suturing there is increasing interest in the use of biological prostheses (allografts/xenografts) and synthetic absorbable meshes.
References :
1- David Rae, Robert Hawthorn (2002) -Sacrocolpopexy for vaginal vault prolapse: a combined vaginal and laparoscopic approach -Gynaecological Endoscopy 11 (2-3), 75-79 .
2- "Uterine Prolapse," eMedicine fromWebMD. www.emedicine.com.
3- Richard S. Bercik, MD, New techniques for correcting vaginal apical prolapse, Contemporary OB/GYN Technology , Originally published: April 15, 2005.
4- Mourtzinos A , Raz S .Lahey Clinic Medical Center, Institute of Urology, Burlington, MA 01805, USA : Curr Opin Obstet Gynecol 2006 Oct;18(5):555-9 . mourtzinos13@yahoo.com
5 -Wattiez, A et al: Promontofixation for the Treatment of Prolapse. Urologic Clinics of North America . Volume 28, Number 1, February 2001; pp. 151-15 .
6-De Lancy J O . Anatomic aspect of vaginal eversion after hysterectomy. AmJ Obstat Gynacol 1992;166:1717-28.
7-Richardson AC. The anatomic defects in rectocele and enterocele.J pelvic surg 1995;4:214-21.
8- Deval B , Haab F . What's new in prolapse surgery?-Department of Gynecology Hospital Beaujon, Clichy , France - : Curr Opin Urol. 2003 Jul;13(4):315-23
9- Benson JT, Lucente V, McClellan E. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol . 1996;175:1418-1422
10-Miklos JR , Kohli N, Lucente V, Saye WB. Site specific fascial defect in the management of enterocele. AMJ obstat gynacol.1998;179:1418-23.
11-Baden WF, Walker T. The anatomy of uterovaginal support . In Baden WF, Walker T, editors surgical repair of vaginal defects. Philadelphia , PA ; JB lippincott company ;1992:25-50.
12-: Richard S. Bercik, MD -Contemporary OB /GYN Technology-Originally published: April 15, 2005
13- SzeEHM, KarramMM.Transvaginal repair of vault prolapse: a review.Obstet Gynecol.1997;89:466-475..
14- Leron E, Stanton SL. Sacrohysteropexy with synthetic mesh for the management of uterovaginal prolapse. British Journal of Obstetrics and Gynaecology 2001;108:629-633..
15 - Beer M , Kuhn A , Bürgerspital Solothurn, Gynacology and Obsterics, Schongrunstrasse 42, 4500 Solothurn , Switzerland. mbeer_so@spital.ktos.ch . Surgical techniques for vault prolapse: a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2005 Apr 1;119(2):144-55.
16-Reda Afifi,Ayman T Sayed - posthysterectomy vaginal vault prolapse-The obstetrician and gynecologist-2005:7:89-97
17-Yatin Thakur, Rajiv Varma .The management of posthysterectomy vaginal vault prolapse using posterior intravaginal sling plasty, the obstetrician and gynecologist, 2005;7:195-198.
18- Dr. Jim W. Ross- Laparoscopic Sacrocolpopexy for Severe Vaginal Prolapse Center for Female Incontinence-Salinas , California .
19- DANIEL H. BILLER, MD, AND G. WILLY DAVILA, MD Vaginal vault prolapse:Identification and surgical options , CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 72 . SUPPLEMENT 4 DECEMBER 2005; 512-519.
20-ShullBL, CapenCV, RiggsMW.Preoperative analysis of site specific pelvic support defects in 81 women treated with sacrospinous ligament suspension and pelvic reconstruction.Am J Obstet Gynecol.1992;166:1764-1771.
21- MeeksGR, WashburneJF, McGehrerRP.Repair of vaginal vault prolapse by suspension of the vagina to iliococcygeus (prespinous) fascia.Am J Obstet Gynecol.1994;171:1444-1449.
22- Maher CF , Murray CJ, Carey M P, Dwyer P I, Ugoni A M. Iliococcygeus or sacrospinous fixation for vaginal vault prolapse, Obst Gyn,2001;98:40-44.
23- Farnsworth BN. Posterior intra vaginal slingplasty (infracoccygeal sacropexy) for severe posthysterectomy vaginal, vault prolapse - a preliminary report on efficacy and safety. Int , Urogynecol J Pelvic Floor Dysfunct 2002; 13 :4-8.
24- SzeEH, KohliN, MiklosJR, RoatT, KarramMM.A retrospective comparison of abdominal sacrocolpopexy with Burch colposuspension versus sacrospinous fixation with transvaginal needle suspension for the management of vaginal vault prolapse and coexisting stress incontinence.Int Urogynecol J Pelvic Floor Dysfunct.1999;10:390-393.





