
Dr Ghulam Hazrat
MBBS; MD; D.MAS
General surgeon at Hirat Regional Hospital Afghanistan
Hirat University Medical School
Member of World Association of Laparoscopic Surgeons
Dr. K. MISHRA, M.MAS; MRCS;
Senior Consultant Laparoscopic Surgeon
Director, World Laparoscopy Hospital, Gurugram, NCR Delhi
Member World Association of Laparoscopic Surgeon
Member Indian Association of Gastrointestinal Endosurgeons
Member Society of American Gastrointestinal and Endoscopic Surgeons
Project submitted towards completion of Diploma in Minimal Access Surgery, World Laparoscopy Hospital, Gurugram, NCR Delhi, INDIA. AUGUST 2007
ABSTRAC
In present article, the usefulness of laparoscopy in diagnosis and treatment of undescended testis is discussed.
Undesended testis is one of the disorders which is common among children in childhood urology.
Here in the initial experience in laparoscopy management of undescended testis will be presented. Laparoscopy was performed on thirteen patients under general anaesthesia , the inguinal canal has been dissected if vas deferens and the internal spermatic vessel made the ways into the internal inguinal ring , orchiopexy or orchiotomy has been performed laparoscopically in cases of intra abdominal testis.
If the internal spermatic vessles has been found terminated interaperetoineal with a blind end the case is going to be considered as a vanishing testis, 13 boys who have been identified with twenty one impalpable testis were between 18 months up to twenty five years ( median 9.8 years ) fourteen of the twenty one impalpable testis , the vessel and vas deferens were seen through the internal ring and the inguinal region needed dissection and then orchiopexy was performed on twelve testis and orchioctomy was performed on two atrophic testis laparoscopically . Four of the twenty one of the testis were found intra abdominal and were localized . Orchiopexy has been performed laparoscopically on two testis and orchiectomy has been performed in two testis laparoscopically and two have been diagnosed vanishing testis and the one which was absence found unilateral on the left side in one of the cases and in the other found bilateral. Laparoscopy is an excellent and help full for diagnostic parposes as well and laparoscopy is the best technique in the diagnosis of undescended testis especially when sonography, C T scaning, MRI are not informative enough.On the other hand orchiopexy and orchiotomy can be done in patients via laparoscopy in intra abdominal testis so the laparoscopy has the most effective and important role in the treatment and diagnosis of the undescended testis.[2,3,6,9,23,42,]
Aim of Study:
Aim is to examine and valuate the role of laparoscopy management of undescended testes.
Key Words:
Diagnostic Laparoscopy, laparoscopy , undescended testis
Introduction:
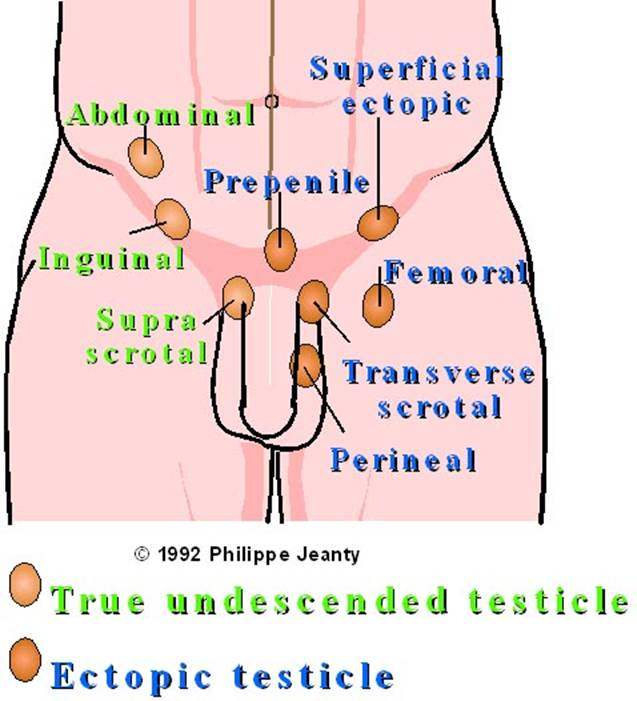
Undescended testis is one of the common genital anomalies in the genital system of boys, and is high in the premature boys comparing to term new borns. In the eigh week of intrauterine life, the testis arise in the abdomen cavity, and descend through inguinal canal to the scrotum in the third trimester.[1] Around 20 % of undescended testis are not palpable[2]. Diagnosis and therapeutic challenges the surgeon and raise the potential of gonads to undergo malignant formation and finally to infertility[3,5]. It is so important to determine the presence or absence of testis,ultra sonography and coputer tomography fail to show undescended testis mostly.Radiology images and open surgical exploration have provide to be not reliable in detecting undescended testis[4,3,2] and finally the laparoscopy has become to have the most important roll in both diagnostic and treatment of undescended testis[4,5]. Before laparoscopy was advented, surgical exploration was used often to show undescended testis but then with laparoscopic technique is used widely in both diagnosis and treatment of undescended testis[6].

Sign: Testicles are the male reproductive organs that produce sperm and the male hormone, testosterone. One or two testicles will not be present in the scrotom during examinations and the testicles might or might not be on the abdominal cavity[2]. In most of boys, undescended testicle descends into the scrotum by itself only. When the testicle doesn't descend, then we recommend surgery after the first year of life experience with undescended testes has showed that outpatient surgery is safe and effective, with excellent outcomes.
Symptoms: Usually no symptoms is present other then inability to find the testicle in the scrotum but in adult infertility will be reported due to undescented testis[2,4].
Problems associated with undescended testis includes the following:
- Infertility
- Inguinal hernia
- Tumor of testicular
- Cosmetic problems and psychological
- Injury of the undescended testis and torsion or twisting of the testis
Material and Methods:
The records on a group of boys who went under diagnostic laparoscopic from 16 patients with 20 undescended testis were found[7] , the data which is collected contains the following , affected side age of the patients ,location of the testis at the time of laparoscopy, operation performed ,complications and the surgeon who performed the surgery. A day before the surgery a clear diet is started and 4-8 hours fasting is required based on the age of the patients and Cefazolin Sodium 40mg/Kg is given to the patient via IM. Physical examination should be done to see if the testis is palpable before the laparoscopy under general anesthesia then the patients is catheterized only if the bladder was palpable. In patient should be in Trendelenbureg position and an incision is made in to the peritoneum and Hasson 5mm blunt trocar was inserted into peritoneum under vision of the telescope and then the abdomen was insufflated with carbon dioxide with pressure of 10 mm Hg and then palpation on the abdomen was done and the abdomen was laparoscopically inspected to rule out any injury and then specific attention to the landmarks ,the location of the length of vas deferens , testicular location and vessels and the presence of a patent processus vaginalis, and volume of the testis,particular anomalies , presence of inguinal hernia were determined[5,7,9] If the testis were found in the abdomen then the size of the testis , mobility ,distance between two testis , appearence, size , length of spermatic vessels and should be also seen and checked and then two more ports inserted , 5 mm in iliac fossa and the other suprapubicaly , in case if the testis was found atrophic then a 10 mm port was inserted and testis was mobilised and gonado vessel disected and clipped and then with a 5 mm trocar which is inserted through the scrotom and then the testis is pulled down. In case if the undescended testis is bilateral an other 10 mm trocar should be inserted on the midclavicular line just bellow the costal margin and then the laparoscopy procedure was performed based on the findings.[7,8,9,10,11,12,13,17,18]. Radioisotope scanning to determine the testis position and its viability is the post operation evaluation[1314,15,16]
Result:
Laparoscopy was performed on thirteen patients who were between eighteen months to 25 years old and 21 impalpable testes were found, from the above mentioned number of patients 9 were in stage of prepubertal , 4 of the patients were in stage of post pubertal, in all these cases the inguinal ring has been seen explored and spermatic vessels and vas deferens were found through the internal ring (66%). In surgical exploration , in 12 testes orchiopexy was performed (57%),and in two testes orchioctomy was performed. On those that the testes were atrophic (9.5%) and on the rest of two (15.4%) beside orchiopexy the repair of inguinal hernia was performed as well. No intra operative compalications were seen , there was not major blood loss during the surgery the operation time was mainly 20 minutes for diagnostic and a mesh was needd for the repair of inguinal hernia which was inserted , the patients were discharged during the next two days from the hospital , even those who were under laparoscopic orchiopexy or orchiotomy have been discharged form the hospital during the first twenty four hours and satisfactory result was achieved . No post operative complications reported in all the above mentioned patients[18,19,20]
Discussion:
Cortesi has used laparoscopy for the first time for diagnose of impalpable undescended testis in 1976 and later on Lowe has reported a large number series of impalpable testis in laparoscopy cases.Since 1990 laparoscopy has been used by urologist for the treatment of impalpable tetis and since then orchiopexy and orchiectomy have been used laparoscopically[1 ,2,3,4,5,6,7] Undescended testis among the paediatric ages group is the significant problem and can be well established and managed orchidopexy by laparoscopy[1,4,7,23,25,26,27,28]
Literature in laparoscopy shows that the accuracy rate of the location of the testis is more then 95% in laparoscopy.Laparoscopy has been help in localize testis and the operation guided by laparoscopy safely and can be used for all ages group. Perinatal torsion is usually cause in absence of testes It is obligatory to assess infuinal canal if spermatic vessels are through the inguinal canal and these vessels might extend to a testis which can be small and might remain in seminiferous tubules and removal must be done in time. laparoscopy has been seen to established as the most reliable diagnostic and treatment management for undescended testis.The anatomy can be demaonstrated clearly and visual information can be provided by laparoscopy which a definite decision will be made.[3,4,5,7,9,11].
A proper introduction of the neddle and telescope is the great help for reaching the proper diagnose in undescended testis sweft and less traumatic.
All other modalites used for diagnostic like ultrasonography, computerized tomography ,resonance and venography have never been as accurate as laparoscopy and are not reliable especially in cases which are reported negative [24,25,26,27] .
We prefer not to try to reduce the testis via scrotal incision and then and artery forceps has been introduced in the internal ring this is found more traumatic and not very simple . In case if the testis could not be broght to the base of the scrotum then it is wrapped it in a silastic membrane and six mounts and then re explored.If the testis was above the internal ring and associated woth closed internal ring then ligation of the testicular vessels with metal clip is recommended without dissecting aggressively at this stage[26,27,28] and after six mount the testis can be brought to the scrotal base which the artery vessal will be developed well.
Laparoscopy is remained the modality of choice for the surgical management anddiagnosis of undescended testis which can be achieved 100% accurate. Atrophic testis should be removed in laparoscope , finally laparoscopy become the methode of choice for diagnosis as well instead of costly investigation like MRI and computer tomography and also prevent unnecessary laparotomy and inguinal exploration[29,30,31].
Complications rarely is reported in diagnostic laparoscopy as the interior wall of the abdomen in children is thinner comparing with adults and this is why the complication is higher in children especially when an un appropriate Veress needle is used , the intestines and vessels might be damaged during insufflations or during the insertion of needle.This is why the complication rarely occurs in patients, no damages have been observed by us how ever leakage CO2 in quite in a few cases to preperitoneal and changing in direction of the needle and formed an appropriate pneumoperitoneum has been reported[16,19.24]. In order to prevent this complication , Hasson method is required and those who had previouse abdominal surgeries but for other cases where is no scar and the risk of the complication is low, Hasson technique is not preferred.
In adult, orchiectomy is the choice of treatment, in cases of unpalpable testis unnessessary surgical intervention can be avoided by laparoscopy, helps to localizes the testis and determine paratesticular pathologies and an appropariate surgical procedure can be selected and orchiopexy performed safely and unnessesary operation can be avoided [6,9,13,24,25,26]
If comparing the operation time, laparoscopically is usually longer then open, operation but with experienced hand the duration can be shortened.
And, finnaly laparoscopy is the most important in diagnosis and treatment of undescended testis and has its own advanteges like less complication rate, less severe post operative pain shorter stay in the hospital, less scar and early return to normal activities [12,13,16,23,26,27].
Conclusion:
Laparoscopy has been found low risk, excellent diagnostic and the the best tool for the management of undescended testis ,with excellent imaging which does not need costly investigations like computerized tomography and MRI. Laparoscopy has been reported as the safest procedure for management of undecended testis , We recommend its routine use for the diagnosis and treatment of undescended testis,
If laparoscopy examination is unsatisfactory for some reason then exploration is still indispensable for the management of undescended testis.
REFERECES:
- Russell RC,Norman SW, Christopher JK. The testis and scrotom. In:Bailey and Loves Short practice of surgery .23rd edn. London: Arnold: 2000.pp.1270-83.
- Craig AP , Louice RK. Laparoscopy in children and adults . In: Patrick CW, Alan BR, duracott E ,Alan JW, ,editors. Campbell’s urology.7th edn. Philadelphia :WB , Saunders Company :1998.pp.2875-911.
- Van Savage JU. Avoidance of inguinal incision in laparoscopically confirmed vanishing testis syndrome , J Urol 2001;166:1421-4.
- Godbole PP Najmaldin AS Laparoscopic orchiodopexy in children, J Endourol 2001.15:251-6
- Tsujihata M, Miyak O,Yashimura k, MAtsumiya k , TakaharaS,etal. Laparoscopic diagnosis and treatment of nonpalpable testis. Int J Urol 2001,8,692-6.
- Docimo S G, Peters C, A,Pediatric endourology and laparoscopy ,in : Campbel Urology Walsh P. C. Retik A, B,Vaughan ED Wein A J Philadephia 2002 pp 2564-2592.
- Storey D W,Mac Kinnon Ak . the laparoscope and the undescended testis J Pediatric Sur 1992,27:89,92.
- Gill B , Kogan S,Starr S,Reda E,, Levitt S,S.Significance of epididymal and ductal anomalies assodiated with testicular maldescent .J Urol 1989. 142.556.8.
- Jacob R . congenital anomalies of the testis and scrotum. In : Patrick C W , Alan BR , E, Duracott E , Alan JW, Editors. Campbell;s Urology. 7th edn. Philadelphia;WB . Saunders company; 1998.pp.2172-92.
- Lee JK , MCClennan BL, Stanley RJ, Sugel SS. Utility of computed tomography in the localization of the undescended testis. Radiology1980;135-121-5.
- Wolverson MK , Houttuin E, Sundaram M , ShieldsJB. Comparison of computed tomography with high resolution real time ultrasound in the localization of the impalpable testis . Radiology 1983; 146:133-6.
- Gill I S , Ross J, H ,Sung, G,T,Kay R, Needlescopeic surgery for cryptorchidism :the initial series . J Pediatr Surg , 2000, 35 (10):1426-1430.
- Kim C, Bennett N , Docimo SG (2005) Missed testis on laparoscopy despite blind – ending vessels and closed processus vaginalis. Urology 65:1226e7-1226e8.
- Schneck F. X,Bellinger M, F . Abnormalities of the testis and scrotum and their surgical management . In: Campbell;s Urology. Walsh P.C, Retik A.B, Vaughan E.D.Wein A . J (eds.) 8th Ed,Saunders company , Philadelphia, 2002.pp 2353-2394.
- KOGAN ,S,J, Hadziselimovic ,F, Howards S,S, Huff, D , Snyder, H,M , Pediatric , Andrology. In :Adult and pediatrict urology .Gillenwater J.Y , Grrayhack J.T. Howard S,S , Mitchell , M. E.(eds.) Fourth Ed , Lippincott . Williams and Wolkins, Philadelphia,2002,pp 2565-2621.
- Cortesi N, Ferrari P, Zambarda E, Manent A, Baldini A, Morano F.P : Diagnosis of bilateral abdominal cryptorchidism by laparoscopy. Endoscopy , 1976,8(1):33-34.
- Brock J. W, HolcoMB, G.W, Morgan W,M,. the use oflaparoscopyin the management of the nonpalpable testis. J laparoendosc sur, 1996, 6,: 35-39.
- Lindgren B. W, Darby E ,C, Faiella L, et , al . laparoscopic orchiopexy: procedure of choice for the nonpalpable testis. J . Urol, 1998. 159 (6):2132- 2135.
- MOORE R.G, Peters C. A, Bauer S. B, Mandell J, Retik A. B. laparoscopic evaluation of the non palpable testes : a prospective assessment of accuracy J Urol , 1994,151 (3):728-731.
- Holcomb G. W, Brock J,W,, Neblett W.W. Ed al. laparoscopy for the non palpable testes . Am Surg.1994. 60 (2): 143-147.
- Cortes, D, Thorup JM, Lenz K , Beck BL , Nielsen OH. Laparoscopy in 100 consecutive patients with 128 impalpable testes. Br J Urol 1995; 1995 ;75:281-7.
- Dean GT,O, reilly PH , brough WA. Laparoscopy for undescended testis: embryological considerations . Br J Urol 1995:76:806- 7.
- De Fillippo RE, Barthold JS,Gonzales R. the application of magnetic resonance imaging for the preoperative localization of non palpable testis in obese children :an alternative to laparoscopy . J Urol 2000: 164: 154-5.
- Lojanapiwat B, Soonthrnpun S, Wudhikarn S. Preoperative laparoscopy in the management of the nonpalpable testis . J Med Assoc Thai 1999; 82:1106-10.
- Hauser R, Lessing JB , Samuel D, Yavetz H, Peyser MR, Paz GF, Hommonnai Z. management of bilateral non palpable testis : laparoscopy diagnosis and orchidectomy. Int J Androl1994; 17:74-7.
- El Gohary MA . The role of laparoscopy in the management of impalpable testis. Pediatr Surg Int 1997; 12:463-5.
- Elder JS. Two-stage Fowler-Stephens orchiopexy in the management of intra – abdominal testes. J Urol 1992, 148:1239-41.
- Yu TJ, Lai MK , Chen WF, Wan YL.Two-stage orchiopexy with laparoscopic clip ligation of spermatic vessels in prune-belly syndrome. J Pediatr Surg 1995,30:870-2.
- Youngson GG , Jones PF . Management of the impalpable testis: Long-term results of the preperitoneal approach. J Pediatr Surg, 1991;26:618-20.
- Merguerian PA , Mevorach RA , Shortliffe LD, cendron M.laparoscopy for the evaluation and management of the non palpable testis. Urology1998;51( Suppl 5 A):3-6.
- Sousa A, Gayoso R,Lopez- Bellido D, Rebordeo J, Perez –Valcarcel J, Fueintes M. Laparoscopic assessment and orchidectomy for adult undescended testis. Surg laparosc Endosc Percutan Tech 2000;10:420-2.
- Roque MC, Fernandez GI,Param de Santiago P, Garcia – cuerpo E, Lavaco Castello F (1993) laparoscopic signs of testicular absence. Arch Espan Urol 24: 233-235.
- cromie WJ (1978) congenital anomalies of the testis , vas, epididymis and inguinal canal.Urol clin North Am 5: 237-257.
- Poenaru D,Homsy YL,Peloqui F, Andze GO(1994) the value of laparoscopy in the diagnosis and treatment of non-palpable testicular cryptorchidism .prog Urol 4:206-273.
- Lowe D.H, Broch W.A. Kaplan G.W. Laparoscopy for localization of non palpable testis.J Urol,1984,131.(4):728-729.
- Poenaru D, laparoscopic management of the impalpable abdominal testis. Urology 1993; 42:574-8.
- lindgren BW , et al. laparoscopic orchidopexy procedure of choice for the nonpalpable testis Urol 1998 ; 159:2132-5.
- Mark SD Davidson PJT. The role of laparoscopy in evaluation of the impalpable undescended testis. Aust NZ J Surg 1997 ; 67:332-4.
- Gill, B Kagon S , Stars , Reda E, Levitt S . significance of epididymal and ductal anomalies associated with testicular maldescent J , Urol;1989; 142;556-8.
- Jordan GH, Winslow BH Laparoscopic single stage and staged orchidopexy J Urol .1994; 152, 1249.
- Thomas R , David AB Arnold C surgery of scrotom and testis in children in Patrick CW , Alan BR Duracott E , Alan JW, Editors. Campbells Urology 7th Edn. Philadelphia WB Saunders Company: 1998 2193-209 pp.
- Van Savage JU. Avoidance of inguinal incision in laparoscopically confirmed vanishing testis syndrome, J Urol 2001.166,142-4.
- Tsujihata M, Miyake O, Yashimura K, Kakimoto K , Matsumiya K , Takahara S , etal . Laparoscopic diagnosisand treatment of nonpalpable testis . Int J Urol 2001, 8: 692-6.
- Bloom Da (1991) Two step orchiopexy with pelvicopic clip ligation of the spermatic vessels . J Urol 145:1030-1033.
- Ronsley PG, voremark JS , Caldmone AA, bellinger MF (1984) Primininary ligation of the gonadal vessels prior to orchidopexy in the intra abdominal testicle : a staged Fowler – stephens procedure . world J Uro 2: 266-268.
- Ivanove A , Dewey C, Fahenkamp D , Luning M(1994) MRIT in non palpable testis. Fortschr Geb Rontgenstrahlen Neuen Bildgeb Verfah 160:249-253.
- Nassar A H M (1995) Laparoscopy assisted orchiopexy : a new approach to the non palpable testis. J Pediatr Surg 30: 39-40.
- Maghnie M , Vanzulli A , Paesano P , Bragheri R, Palladini G preti P , et al . the accuracy of magnetic resonance imaging and ultrasonography compared with surgical findings in the localization of the undescended testis .Arch Pediatr Adolesc Med 1994; 148:699-703.
- Rajfer J , Tauber A ,Zinner N, Naftulin E,worthen N , the use of computerized tomography scaning to localize the impalpable testis . J Urol 1983;129:972-4.
- Antony Ac . Laparoscopy and the management of the non palpable testis . In Thomas RG , Mark AT , John LL, editors . laparoscopy surgery, first Indian Edn. New delhi Jaypee brothers , 1994.pp 161-70.
- Riquelme M(2002) Laparoscopic orchiopexy for the palpable and non palpable undescended testis (submitted).In: Presented at the amirican academy of pediatrics 2002 national conference and exhibition , October ,pp .18-23 , Boston ( urology section).
- Glenn J F (ed)(1991) Urologic surgery ,4th edn. Lippincott, Philadelphia.





