Page 10 - World Journal of Laparoscopic Surgery
P. 10
Piyush Singhania et al
open and took 4 hours. The operative time decreased with
surgeons experience. Average operating time for first 7 cases
was 4.36 hours and it decreased to an average of 3.14 hours for
the next 7 cases excluding 1 case which needed conversion to
open. Mean blood loss was 150 ml (range 70-250 ml). None of
our patients required any blood transfusion. Average amount
of gas used was 230 L (range 127-480 L). The mean duration of
analgesic use in our series was 5.2 days (ranging from 3 days to
10 days) excluding 2 patients who required open surgery. Mean
hospital stay after surgery was 7.6 days (range 3-23 days).
However, if two cases which required open surgery were
excluded the mean hospital stay, after surgery was 5.5 days
(range 3-9 days).
There was one case of accidental division of upper end of
A
DJ stent during pelvic transection. The upper end was
subsequently removed and the rest of the stent left in situ. An
eight years old child had very fragile pelvic and ureteral tissues
and there was repeated cut through of sutures during uretero
pelvic anastomosis. In this child, the procedure was converted
to open approach and pyeloplasty completed. Removal of
associated calculus was done in 3 out of 4 patients but clearance
was achieved in only one patient who had a pelvic calculus.
Rest of the patients with calyceal calculi which could not be
retrieved were advised ESWL postoperatively. Our second
patient had postoperative urinary extravasation and urinary
peritonitis. She required abdominal exploration with interrupted
suturing of anterior suture line and PCN on 7th postoperative
day. Subsequently the recovery was uneventful.
Follow-up ranged from 4 months to 16 months. Mean follow-
up period was 10.6 months. 4 (26.7%) out of 15 patients
continued to complaints of intermittent flank pain inspite of
radiological evidence of definite improvement in drainage. One
B patient had no improvement in symptoms and persistence of
radiologic evidence of obstruction. This patient had gross HN
with nil cortical thickness preoperatively.
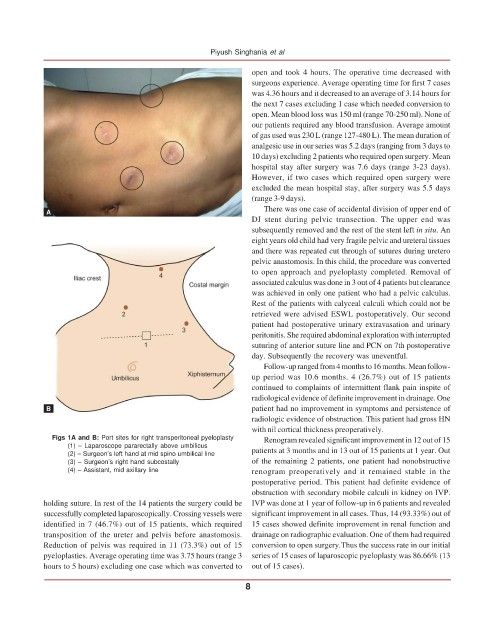
Figs 1A and B: Port sites for right transperitoneal pyeloplasty Renogram revealed significant improvement in 12 out of 15
(1) – Laparoscope pararectally above umbilicus patients at 3 months and in 13 out of 15 patients at 1 year. Out
(2) – Surgeon’s left hand at mid spino umbilical line
(3) – Surgeon’s right hand subcostally of the remaining 2 patients, one patient had nonobstructive
(4) – Assistant, mid axillary line renogram preoperatively and it remained stable in the
postoperative period. This patient had definite evidence of
obstruction with secondary mobile calculi in kidney on IVP.
holding suture. In rest of the 14 patients the surgery could be IVP was done at 1 year of follow-up in 6 patients and revealed
successfully completed laparoscopically. Crossing vessels were significant improvement in all cases. Thus, 14 (93.33%) out of
identified in 7 (46.7%) out of 15 patients, which required 15 cases showed definite improvement in renal function and
transposition of the ureter and pelvis before anastomosis. drainage on radiographic evaluation. One of them had required
Reduction of pelvis was required in 11 (73.3%) out of 15 conversion to open surgery.Thus the success rate in our initial
pyeloplasties. Average operating time was 3.75 hours (range 3 series of 15 cases of laparoscopic pyeloplasty was 86.66% (13
hours to 5 hours) excluding one case which was converted to out of 15 cases).
8