Page 4 - WJOLS
P. 4
Sherif Z Kotb et al
or marked bleeding tendency with prothrombin time more than Laparoscopic Intraoperative Ultrasound (IOUS)
3
50% and a platelet count more than 100000/mm . With absence Assessment
or minimal ascites.
An ultrasound probe was inserted through the second trocar
Surgical Technique to assess any radiographically occult or unablatable disease,
detect any extrahepatic lesion (if present was biopsed), better
Ablation was done by the RF 3000 generator (Radiotherapeutics) declaration of the number and location of liver tumours, and
with a power of up to 200 W and 7 electrode prongs. Maximum decide the puncture point (Fig. 2).
power output of the RF generator, amount of electrode array
deployment from the trocar, and duration of the effective time Ultrasound-guided Laparoscopic RF Ablation
of the ablation were established at the beginning of the
procedure with the goal of destroying the visible tumour mass The RF electrode was accurately placed into the tumour, without
plus a 0.5 to 1 cm safety margin all around. puncturing the nearby blood vessel (under the ultrasonic
guidance). We indirectly puncture of the tumour by the RF
Laparoscopic Assessment electrode through non-tumourous liver parenchyma, to avoid
needle track seedling, (Fig. 3). The tip of the needle (with
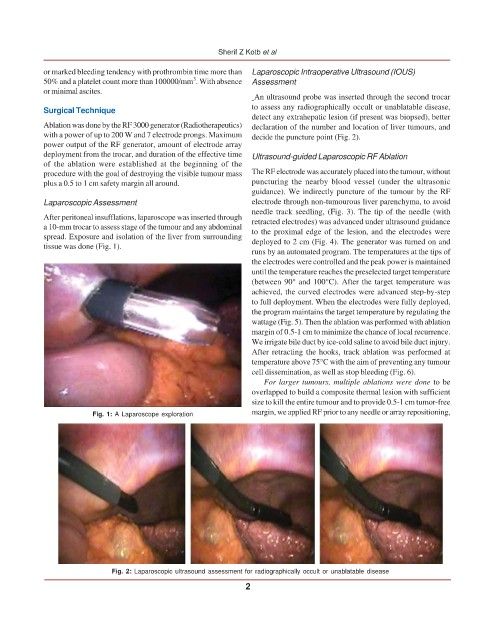
After peritoneal insufflations, laparoscope was inserted through retracted electrodes) was advanced under ultrasound guidance
a 10-mm trocar to assess stage of the tumour and any abdominal to the proximal edge of the lesion, and the electrodes were
spread. Exposure and isolation of the liver from surrounding deployed to 2 cm (Fig. 4). The generator was turned on and
tissue was done (Fig. 1).
runs by an automated program. The temperatures at the tips of
the electrodes were controlled and the peak power is maintained
until the temperature reaches the preselected target temperature
(between 90° and 100°C). After the target temperature was
achieved, the curved electrodes were advanced step-by-step
to full deployment. When the electrodes were fully deployed,
the program maintains the target temperature by regulating the
wattage (Fig. 5). Then the ablation was performed with ablation
margin of 0.5-1 cm to minimize the chance of local recurrence.
We irrigate bile duct by ice-cold saline to avoid bile duct injury.
After retracting the hooks, track ablation was performed at
temperature above 75°C with the aim of preventing any tumour
cell dissemination, as well as stop bleeding (Fig. 6).
For larger tumours, multiple ablations were done to be
overlapped to build a composite thermal lesion with sufficient
size to kill the entire tumour and to provide 0.5-1 cm tumor-free
Fig. 1: A Laparoscope exploration margin, we applied RF prior to any needle or array repositioning,
Fig. 2: Laparoscopic ultrasound assessment for radiographically occult or unablatable disease
2