Page 6 - World Journal of Laparoscopic Surgery
P. 6
Bhanu P Sharma et al
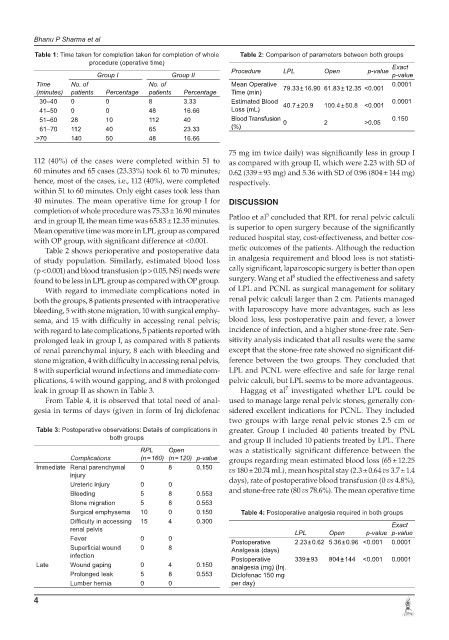
Table 1: Time taken for completion taken for completion of whole Table 2: Comparison of parameters between both groups
procedure (operative time)
Procedure LPL Open p-value Exact
Group I Group II p-value
Time No. of No. of Mean Operative 79.33 ± 16.90 61.83 ± 12.35 <0.001 0.0001
(minutes) patients Percentage patients Percentage Time (min)
30–40 0 0 8 3.33 Estimated Blood 40.7 ± 20.9 100.4 ± 50.8 <0.001 0.0001
41–50 0 0 48 16.66 Loss (mL)
51–60 28 10 112 40 Blood Transfusion 0 2 >0.05 0.150
61–70 112 40 65 23.33 (%)
>70 140 50 48 16.66
75 mg im twice daily) was significantly less in group I
112 (40%) of the cases were completed within 51 to as compared with group II, which were 2.23 with SD of
60 minutes and 65 cases (23.33%) took 61 to 70 minutes; 0.62 (339 ± 93 mg) and 5.36 with SD of 0.96 (804 ± 144 mg)
hence, most of the cases, i.e., 112 (40%), were completed respectively.
within 51 to 60 minutes. Only eight cases took less than
40 minutes. The mean operative time for group I for DISCUSSION
completion of whole procedure was 75.33 ± 16.90 minutes 5
and in group II, the mean time was 65.83 ± 12.35 minutes. Patloo et al concluded that RPL for renal pelvic calculi
Mean operative time was more in LPL group as compared is superior to open surgery because of the significantly
with OP group, with significant difference at <0.001. reduced hospital stay, cost-effectiveness, and better cos-
Table 2 shows perioperative and postoperative data metic outcomes of the patients. Although the reduction
of study population. Similarly, estimated blood loss in analgesia requirement and blood loss is not statisti-
(p < 0.001) and blood transfusion (p > 0.05, NS) needs were cally significant, laparoscopic surgery is better than open
6
found to be less in LPL group as compared with OP group. surgery. Wang et al studied the effectiveness and safety
With regard to immediate complications noted in of LPL and PCNL as surgical management for solitary
both the groups, 8 patients presented with intraoperative renal pelvic calculi larger than 2 cm. Patients managed
bleeding, 5 with stone migration, 10 with surgical emphy- with laparoscopy have more advantages, such as less
sema, and 15 with difficulty in accessing renal pelvis; blood loss, less postoperative pain and fever, a lower
with regard to late complications, 5 patients reported with incidence of infection, and a higher stone-free rate. Sen-
prolonged leak in group I, as compared with 8 patients sitivity analysis indicated that all results were the same
of renal parenchymal injury, 8 each with bleeding and except that the stone-free rate showed no significant dif-
stone migration, 4 with difficulty in accessing renal pelvis, ference between the two groups. They concluded that
8 with superficial wound infections and immediate com- LPL and PCNL were effective and safe for large renal
plications, 4 with wound gapping, and 8 with prolonged pelvic calculi, but LPL seems to be more advantageous.
7
leak in group II as shown in Table 3. Haggag et al investigated whether LPL could be
From Table 4, it is observed that total need of anal- used to manage large renal pelvic stones, generally con-
gesia in terms of days (given in form of Inj diclofenac sidered excellent indications for PCNL. They included
two groups with large renal pelvic stones 2.5 cm or
Table 3: Postoperative observations: Details of complications in greater. Group I included 40 patients treated by PNL
both groups and group II included 10 patients treated by LPL. There
RPL Open was a statistically significant difference between the
Complications (n = 160) (n = 120) p-value groups regarding mean estimated blood loss (65 ± 12.25
Immediate Renal parenchymal 0 8 0.150 vs 180 ± 20.74 mL), mean hospital stay (2.3 ± 0.64 vs 3.7 ± 1.4
injury days), rate of postoperative blood transfusion (0 vs 4.8%),
Ureteric injury 0 0
Bleeding 5 8 0.553 and stone-free rate (80 vs 78.6%). The mean operative time
Stone migration 5 8 0.553
Surgical emphysema 10 0 0.150 Table 4: Postoperative analgesia required in both groups
Difficulty in accessing 15 4 0.300 Exact
renal pelvis LPL Open p-value p-value
Fever 0 0 Postoperative 2.23 ± 0.62 5.36 ± 0.96 <0.001 0.0001
Superficial wound 0 8 Analgesia (days)
infection Postoperative 339 ± 93 804 ± 144 <0.001 0.0001
Late Wound gaping 0 4 0.150 analgesia (mg) (Inj.
Prolonged leak 5 8 0.553 Diclofenac 150 mg
Lumber hernia 0 0 per day)
4