Patient-Specific Instruments in Robotic Surgery: A New Trend
Patient-Specific Instruments in Robotic Surgery: A New Trend
Introduction:
Robotic surgery has witnessed remarkable advancements in recent years, revolutionizing the landscape of medical interventions. Among the latest trends, the integration of patient-specific instruments stands out as a groundbreaking development. This article explores the emergence, benefits, challenges, and future prospects of patient-specific instruments in robotic surgery, shedding light on the transformative potential they hold for personalized and precise medical procedures.
Evolution of Robotic Surgery: A Paradigm Shift
Robotic surgery has evolved significantly since its inception, with the introduction of robotic-assisted systems such as the da Vinci Surgical System. These systems have enhanced surgeons' capabilities by providing improved dexterity, precision, and visualization during minimally invasive procedures. As technology continues to advance, the focus has shifted towards tailoring surgical instruments to individual patients, marking the beginning of a new era in robotic surgery.
Understanding Patient-Specific Instruments
Patient-specific instruments (PSIs) in robotic surgery involve the customization of surgical tools based on the unique anatomy and requirements of each patient. This customization is made possible through advanced imaging techniques, such as CT scans and MRIs, which provide detailed insights into the patient's anatomy. The collected data is then used to design and manufacture instruments that precisely fit the patient's anatomy, optimizing surgical outcomes.
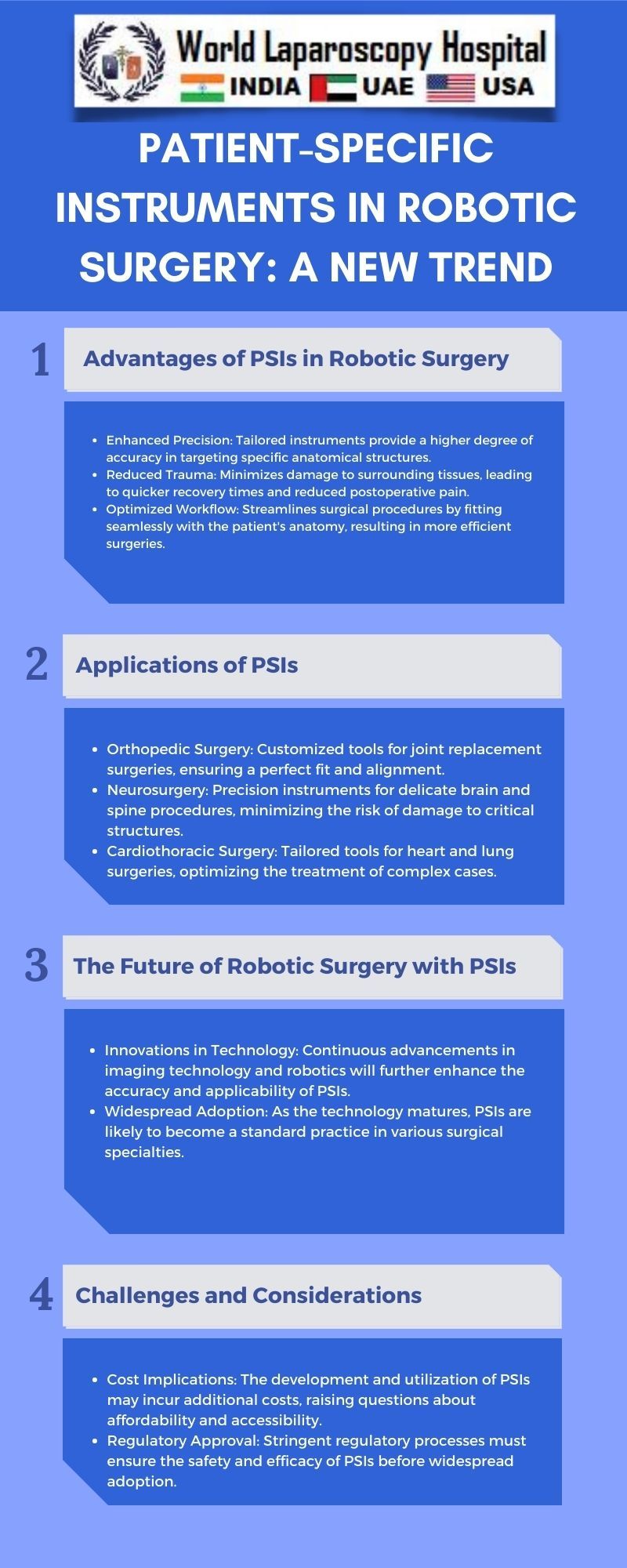
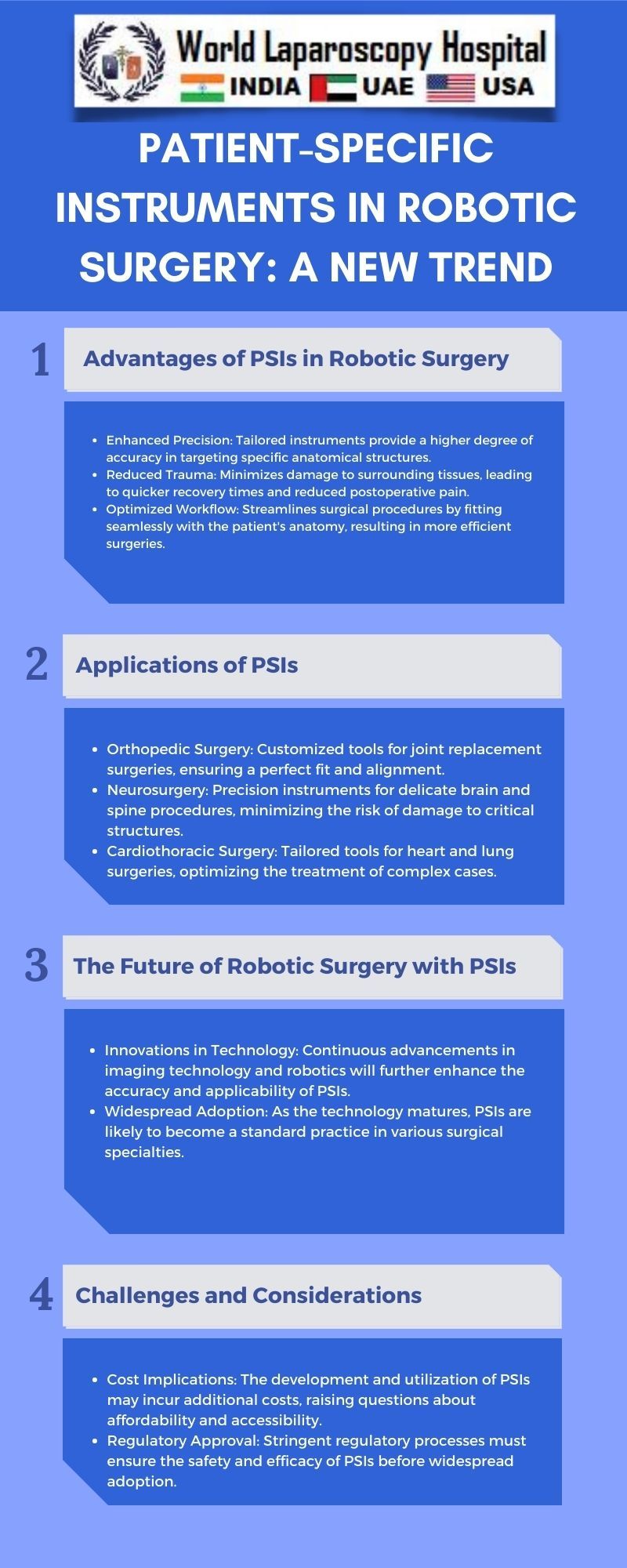
Benefits of Patient-Specific Instruments
Enhanced Precision and Accuracy:
One of the primary advantages of patient-specific instruments is the heightened level of precision they offer. By tailoring instruments to fit the specific anatomy of each patient, surgeons can navigate complex structures with greater accuracy, reducing the risk of damage to surrounding tissues and improving overall procedural precision.
Improved Surgical Efficiency:
PSIs contribute to increased surgical efficiency by streamlining procedures. Surgeons can spend less time adjusting and adapting generic instruments, as patient-specific tools are designed to seamlessly integrate with the unique anatomy of the individual. This efficiency not only saves time but also enhances the overall surgical experience for both the medical team and the patient.
Minimized Trauma and Recovery Time:
The precision afforded by patient-specific instruments can lead to minimized trauma during surgery. Reduced trauma often translates to quicker recovery times and shorter hospital stays for patients. This is particularly significant in minimally invasive procedures, where the goal is to achieve optimal outcomes with minimal impact on the patient's body.
Optimized Surgical Outcomes:
Tailoring instruments to each patient's anatomy allows for a more personalized approach to surgery. This customization contributes to optimized outcomes, as surgeons can adapt their techniques based on the specific characteristics of the patient. This individualized approach is particularly valuable in complex and delicate procedures.
Challenges and Considerations
Technological and Financial Barriers:
The implementation of patient-specific instruments requires advanced technological capabilities, including sophisticated imaging technologies and computer-aided design (CAD) software. Additionally, the associated costs of designing and manufacturing customized instruments may pose financial challenges for healthcare institutions. Addressing these barriers is crucial for widespread adoption.
Standardization and Regulatory Approval:
Achieving standardization in the design and manufacturing processes of patient-specific instruments is a challenge. Regulatory bodies need to establish clear guidelines and standards to ensure the safety and effectiveness of these customized tools. Striking a balance between innovation and regulatory compliance is essential to foster trust in the medical community.
Integration with Existing Systems:
The seamless integration of patient-specific instruments with existing robotic surgical systems is another consideration. Compatibility issues and the need for interoperability between different technologies must be addressed to ensure the smooth adoption of these customized tools in various medical settings.
Training and Education:
The introduction of patient-specific instruments necessitates training healthcare professionals in their use. Surgeons, nurses, and other members of the medical team need to acquire the skills and knowledge required to leverage the full potential of these customized tools. Educational programs and hands-on training sessions are vital to overcoming this challenge.
Case Studies and Success Stories
Neurosurgery:
Patient-specific instruments have shown promising results in neurosurgical procedures, where precision is paramount. Customized tools designed for specific cranial and spinal anatomies have led to reduced complications and improved patient outcomes. The ability to navigate intricate neural structures with enhanced precision has transformed the field of neurosurgery.
Orthopedics:
In orthopedic surgery, patient-specific instruments have been utilized for joint replacement surgeries. Customized cutting guides and implants, tailored to the patient's anatomy, have contributed to improved implant fit, reduced postoperative pain, and faster recovery times. The orthopedic community is increasingly recognizing the value of personalized instrumentation in enhancing the success of joint replacement procedures.
Cardiac Surgery:
Patient-specific instruments have also found application in cardiac surgery, particularly in procedures like valve replacement. Customized tools enable surgeons to navigate the intricacies of the heart with precision, minimizing the risk of damage to surrounding structures. As a result, patients undergoing cardiac surgery may experience reduced postoperative complications and faster recovery.
Future Directions and Innovations
Artificial Intelligence Integration:
The integration of artificial intelligence (AI) in the design and manufacturing processes of patient-specific instruments holds great potential. AI algorithms can analyze vast amounts of patient data, assisting in the creation of highly customized tools. This could lead to more efficient and accurate customization, further improving surgical outcomes.
Expanded Applications:
As technology continues to advance, the scope of patient-specific instruments is likely to expand across various medical specialties. Applications in fields such as urology, gynecology, and general surgery could become more prevalent, offering tailored solutions for a wide range of procedures.
Global Collaboration:
The future of patient-specific instruments may involve global collaboration, with researchers, surgeons, and technology experts working together to refine and standardize the processes. International efforts can help overcome challenges related to standardization, regulatory approval, and technology integration, paving the way for widespread adoption.
Patient Involvement and Awareness:
Increased awareness and involvement of patients in the use of patient-specific instruments are crucial for successful implementation. Educating patients about the benefits and potential risks, as well as involving them in the decision-making process, can contribute to greater acceptance and trust in these innovative surgical approaches.
Conclusion:
The integration of patient-specific instruments represents a paradigm shift in the field of robotic surgery, offering unprecedented levels of precision, efficiency, and personalized care. While challenges exist, ongoing advancements in technology, standardization efforts, and global collaboration are paving the way for the widespread adoption of these innovative tools. As patient-specific instruments continue to redefine the possibilities in surgical interventions, the future holds exciting prospects for personalized and optimized healthcare delivery.
Top
Introduction:
Robotic surgery has witnessed remarkable advancements in recent years, revolutionizing the landscape of medical interventions. Among the latest trends, the integration of patient-specific instruments stands out as a groundbreaking development. This article explores the emergence, benefits, challenges, and future prospects of patient-specific instruments in robotic surgery, shedding light on the transformative potential they hold for personalized and precise medical procedures.
Evolution of Robotic Surgery: A Paradigm Shift
Robotic surgery has evolved significantly since its inception, with the introduction of robotic-assisted systems such as the da Vinci Surgical System. These systems have enhanced surgeons' capabilities by providing improved dexterity, precision, and visualization during minimally invasive procedures. As technology continues to advance, the focus has shifted towards tailoring surgical instruments to individual patients, marking the beginning of a new era in robotic surgery.
Understanding Patient-Specific Instruments
Patient-specific instruments (PSIs) in robotic surgery involve the customization of surgical tools based on the unique anatomy and requirements of each patient. This customization is made possible through advanced imaging techniques, such as CT scans and MRIs, which provide detailed insights into the patient's anatomy. The collected data is then used to design and manufacture instruments that precisely fit the patient's anatomy, optimizing surgical outcomes.
Benefits of Patient-Specific Instruments
Enhanced Precision and Accuracy:
One of the primary advantages of patient-specific instruments is the heightened level of precision they offer. By tailoring instruments to fit the specific anatomy of each patient, surgeons can navigate complex structures with greater accuracy, reducing the risk of damage to surrounding tissues and improving overall procedural precision.
Improved Surgical Efficiency:
PSIs contribute to increased surgical efficiency by streamlining procedures. Surgeons can spend less time adjusting and adapting generic instruments, as patient-specific tools are designed to seamlessly integrate with the unique anatomy of the individual. This efficiency not only saves time but also enhances the overall surgical experience for both the medical team and the patient.
Minimized Trauma and Recovery Time:
The precision afforded by patient-specific instruments can lead to minimized trauma during surgery. Reduced trauma often translates to quicker recovery times and shorter hospital stays for patients. This is particularly significant in minimally invasive procedures, where the goal is to achieve optimal outcomes with minimal impact on the patient's body.
Optimized Surgical Outcomes:
Tailoring instruments to each patient's anatomy allows for a more personalized approach to surgery. This customization contributes to optimized outcomes, as surgeons can adapt their techniques based on the specific characteristics of the patient. This individualized approach is particularly valuable in complex and delicate procedures.
Challenges and Considerations
Technological and Financial Barriers:
The implementation of patient-specific instruments requires advanced technological capabilities, including sophisticated imaging technologies and computer-aided design (CAD) software. Additionally, the associated costs of designing and manufacturing customized instruments may pose financial challenges for healthcare institutions. Addressing these barriers is crucial for widespread adoption.
Standardization and Regulatory Approval:
Achieving standardization in the design and manufacturing processes of patient-specific instruments is a challenge. Regulatory bodies need to establish clear guidelines and standards to ensure the safety and effectiveness of these customized tools. Striking a balance between innovation and regulatory compliance is essential to foster trust in the medical community.
Integration with Existing Systems:
The seamless integration of patient-specific instruments with existing robotic surgical systems is another consideration. Compatibility issues and the need for interoperability between different technologies must be addressed to ensure the smooth adoption of these customized tools in various medical settings.
Training and Education:
The introduction of patient-specific instruments necessitates training healthcare professionals in their use. Surgeons, nurses, and other members of the medical team need to acquire the skills and knowledge required to leverage the full potential of these customized tools. Educational programs and hands-on training sessions are vital to overcoming this challenge.
Case Studies and Success Stories
Neurosurgery:
Patient-specific instruments have shown promising results in neurosurgical procedures, where precision is paramount. Customized tools designed for specific cranial and spinal anatomies have led to reduced complications and improved patient outcomes. The ability to navigate intricate neural structures with enhanced precision has transformed the field of neurosurgery.
Orthopedics:
In orthopedic surgery, patient-specific instruments have been utilized for joint replacement surgeries. Customized cutting guides and implants, tailored to the patient's anatomy, have contributed to improved implant fit, reduced postoperative pain, and faster recovery times. The orthopedic community is increasingly recognizing the value of personalized instrumentation in enhancing the success of joint replacement procedures.
Cardiac Surgery:
Patient-specific instruments have also found application in cardiac surgery, particularly in procedures like valve replacement. Customized tools enable surgeons to navigate the intricacies of the heart with precision, minimizing the risk of damage to surrounding structures. As a result, patients undergoing cardiac surgery may experience reduced postoperative complications and faster recovery.
Future Directions and Innovations
Artificial Intelligence Integration:
The integration of artificial intelligence (AI) in the design and manufacturing processes of patient-specific instruments holds great potential. AI algorithms can analyze vast amounts of patient data, assisting in the creation of highly customized tools. This could lead to more efficient and accurate customization, further improving surgical outcomes.
Expanded Applications:
As technology continues to advance, the scope of patient-specific instruments is likely to expand across various medical specialties. Applications in fields such as urology, gynecology, and general surgery could become more prevalent, offering tailored solutions for a wide range of procedures.
Global Collaboration:
The future of patient-specific instruments may involve global collaboration, with researchers, surgeons, and technology experts working together to refine and standardize the processes. International efforts can help overcome challenges related to standardization, regulatory approval, and technology integration, paving the way for widespread adoption.
Patient Involvement and Awareness:
Increased awareness and involvement of patients in the use of patient-specific instruments are crucial for successful implementation. Educating patients about the benefits and potential risks, as well as involving them in the decision-making process, can contribute to greater acceptance and trust in these innovative surgical approaches.
Conclusion:
The integration of patient-specific instruments represents a paradigm shift in the field of robotic surgery, offering unprecedented levels of precision, efficiency, and personalized care. While challenges exist, ongoing advancements in technology, standardization efforts, and global collaboration are paving the way for the widespread adoption of these innovative tools. As patient-specific instruments continue to redefine the possibilities in surgical interventions, the future holds exciting prospects for personalized and optimized healthcare delivery.
